Generic Drugs: What They Are, How They Work, and When to Choose Them
When you hear generic drugs, pharmaceutical products that contain the same active ingredients as brand-name drugs but are sold without a brand name. Also known as generic medications, they are approved by the FDA to work the same way, in the same amount, and with the same safety profile as their brand-name counterparts. Yet many people still hesitate to use them—wondering if they’re just cheaper copies, or if they might not work as well. The truth? For over 90% of medications, generic drugs are just as safe and effective. The only real difference is the price—and sometimes the shape or color of the pill.
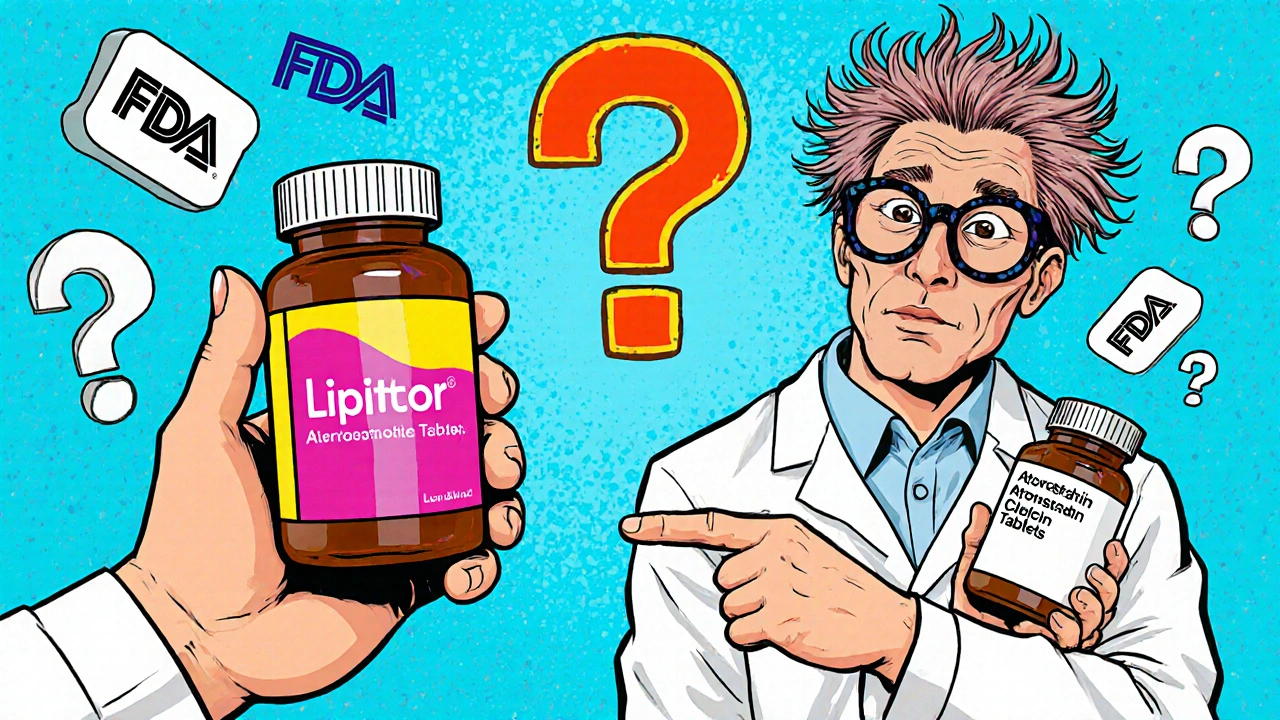
What makes a drug "generic" isn’t its ingredients—it’s the timing. Once a brand-name drug’s patent expires, other manufacturers can produce the same medicine using the same active compound. The FDA requires these generics to meet strict standards: same dosage, same strength, same route of administration, same shelf life, and same performance in the body. That means a generic lisinopril works just like Prinivil. A generic metformin acts the same as Glucophage. You’re not getting a lesser version—you’re getting the same treatment, often at 80% less cost.
But not every situation calls for a switch. Some medications, like warfarin or levothyroxine, need very precise dosing, and even small differences in inactive ingredients can affect how your body absorbs them. That’s why your doctor might recommend sticking with the brand—especially if you’re sensitive to changes. And while most generics are made in the same high-quality facilities as brand-name drugs, some people report different side effects when switching between manufacturers. It’s not the active ingredient changing—it’s the fillers, dyes, or coatings. If you notice a difference after switching, talk to your pharmacist. They can help you find a generic that matches your tolerance.
Understanding FDA approval, the process that ensures generic drugs are bioequivalent to brand-name versions before they hit the market helps cut through the fear. The FDA doesn’t approve generics lightly. They test them in labs, review manufacturing sites, and even check how the drug breaks down in the body. In fact, many brand-name companies make their own generics once the patent expires. The system isn’t broken—it’s designed to save you money without sacrificing safety.
And then there’s medication cost, the biggest reason most people choose generics, especially without insurance or with high deductibles. A 30-day supply of brand-name Lipitor might cost $300. The generic atorvastatin? $10. That’s not a marketing trick—it’s the result of competition. When multiple companies make the same drug, prices drop fast. Online pharmacy counseling services, like those covered in our posts, can help you find the lowest prices on generics, even without insurance.
Some of our articles dive into cases where sticking with the brand makes sense—like when consistency matters for mental health meds or chronic conditions. Others show how to use label information to avoid timing mistakes with fiber supplements or how to spot dangerous interactions with MAOIs. You’ll also find guides on how to read medication guides for overdose warnings, how to build an emergency go-bag with your generics, and how to use drug interaction checkers safely. These aren’t theoretical tips—they’re real strategies people use every day to manage their health without overspending.
Generic drugs aren’t a compromise. They’re a smart choice—for your body and your budget. Whether you’re managing high blood pressure, diabetes, depression, or just trying to cut costs, knowing how to navigate the world of generics gives you real power. Below, you’ll find practical, no-fluff advice from people who’ve been there: pharmacists, patients, and clinicians who’ve seen what works—and what doesn’t—when it comes to saving money without sacrificing care.
How the FDA Ensures Generic Drugs Work the Same as Brands
The FDA ensures generic drugs work the same as brand-name drugs through strict bioequivalence testing, identical active ingredients, and rigorous manufacturing standards. Over 90% of U.S. prescriptions use generics, saving billions annually.

Why Most Drugs Don’t Have Authorized Generics - And What It Means for Your Prescription Costs
Most drugs don’t have authorized generics because drugmakers only create them to protect profits - not to lower prices. Learn why this affects your prescription costs and what you can do.

State Laws on Generic Drug Substitution: How Rules Vary Across the U.S.
State laws on generic drug substitution vary widely across the U.S., affecting how pharmacists replace brand-name drugs with cheaper generics. These rules impact cost, safety, and patient trust-especially for critical medications.

Therapeutic Equivalence Codes: How the FDA Determines Which Generic Drugs Can Be Substituted
The FDA uses therapeutic equivalence codes to determine which generic drugs can be safely substituted for brand-name medications. Learn how the A and B codes work, why some generics aren't interchangeable, and how this system saves billions in healthcare costs.

Stability and Shelf Life: How Generic Products Degrade and Why Safety Matters
Stability and shelf life determine whether generic medications remain safe and effective over time. Learn how degradation happens, why storage matters, and what you need to know to protect your health.
Medication Therapy Management: How Pharmacists Optimize Generic Drug Use for Better Outcomes
Pharmacists play a vital role in Medication Therapy Management by optimizing generic drug use to improve adherence, reduce costs, and prevent adverse events. Learn how MTM works and why it matters for patients on multiple medications.
How to Understand Authorized Generics and How They Differ from Traditional Generics
Authorized generics are the exact same drug as brand-name medications, just without the brand label. Learn how they differ from traditional generics in ingredients, cost, insurance coverage, and how to identify them.




