When you pick up a generic pill from the pharmacy, you assume it works just like the brand-name version. But what happens to that pill over time? Does it stay safe? Does it still work? The answer lies in stability and shelf life - two terms that aren’t just lab jargon, but critical to your health.
What Does "Stability" Really Mean?
Stability isn’t about whether a pill feels hard or looks the same. It’s about whether the active ingredient still does what it’s supposed to do, and whether anything harmful has formed over time. The U.S. Food and Drug Administration (FDA) defines it clearly: a product must retain its chemical, physical, microbiological, and functional properties within strict limits from the moment it’s packaged until its expiration date.That means four things must stay in check:
- Chemical stability: The main drug molecule shouldn’t break down into toxic byproducts. High-Performance Liquid Chromatography (HPLC) tests detect impurities as small as 0.1% - a tiny amount, but enough to cause harm if left unchecked.
- Physical stability: Tablets shouldn’t crack, capsules shouldn’t leak, and suspensions shouldn’t clump. For example, some nanoparticle-based drugs lose effectiveness if particles grow larger than 200 nanometers. That’s smaller than a virus - but big enough to stop them from reaching their target in your body.
- Microbiological stability: No mold, no bacteria. Non-sterile products must stay under 100 colony-forming units per gram. Sterile ones? They must have a 1-in-1 million chance of contamination - a standard so strict it’s designed to protect people with weakened immune systems.
- Functional stability: Inhalers must deliver the exact same dose each time. If a metered-dose inhaler delivers only 85% of its labeled dose after six months, it’s no longer safe to use.
How Do They Test This?
Testing doesn’t happen overnight. The International Council for Harmonisation (ICH) guidelines, specifically Q1A(R2), set the global standard. For most drugs, manufacturers must run long-term studies at 25°C and 60% humidity - conditions meant to mimic a typical home or pharmacy shelf. They test at 0, 3, 6, 9, 12, 18, 24, and even 36 months.That’s right - a drug with a 3-year shelf life needs three full years of real-time testing before it can be approved. But companies don’t wait that long to launch. They use accelerated testing: 40°C and 75% humidity for six months. If nothing breaks down under those harsh conditions, they extrapolate the results to predict stability at room temperature.
Here’s the catch: this extrapolation isn’t foolproof. One quality assurance professional on a pharmaceutical forum lost $250,000 and 18 months because their accelerated test showed zero degradation - but real-time testing revealed crystallization at the 24-month mark. Why? A hidden polymorphic transition. The drug molecule changed its shape under normal conditions, something the high-heat test didn’t trigger.
Why Generic Drugs Are Different
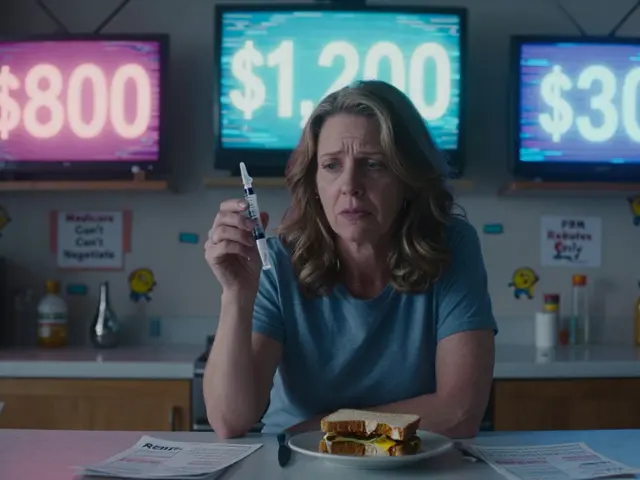
Generic drugs are cheaper because they don’t repeat the expensive clinical trials of the original. But they still must prove bioequivalence - meaning they deliver the same amount of drug into your bloodstream. What they don’t always prove is identical stability.A 2020 FDA study found that 17.3% of generic levothyroxine products had stability issues not seen in Synthroid, the brand-name version. Why? Different fillers, coatings, or packaging. One generic used a less moisture-resistant capsule. Over time, humidity got in. The drug degraded. Patients got inconsistent doses - some underdosed, risking hypothyroidism; others overdosed, risking heart problems.
It’s not just levothyroxine. Similar issues have been found in antibiotics, blood pressure meds, and even insulin. The excipients - the inactive ingredients - matter more than most people realize. A different stabilizer can change how fast a drug breaks down. And if the manufacturer doesn’t test under real-world conditions, you’re the one who pays the price.

Storage Isn’t Optional - It’s Legal
You’ve probably seen “Store at room temperature” on a label. That’s not a suggestion. The FDA requires exact documentation. “Room temperature” isn’t just whatever your house feels like. It’s 15-30°C (59-86°F), and the optimal reference point is 24-25°C. If your medicine sits on a windowsill in summer, or in a hot car, or above a radiator, it’s not just losing potency - you’re breaking the law.And here’s the kicker: 80% of FDA inspection findings related to stability testing involve poor storage documentation. One company got cited because their records just said “stored in warehouse.” No temperature logs. No humidity controls. No proof they even monitored it. That’s not negligence - it’s a failure to protect patients.
What Happens When Stability Fails?
When a drug degrades, it doesn’t just become weak. It can become dangerous.- Aspirin breaks down into acetic acid - you get a vinegar smell. That’s not just unpleasant. It means the painkiller is losing strength.
- Some antibiotics, like tetracycline, degrade into toxic compounds that can damage kidneys.
- Insulin exposed to heat loses potency. Diabetics using degraded insulin risk dangerous spikes in blood sugar.
- For food products, microbial growth isn’t just about spoilage - it’s about botulism, salmonella, listeria. One failed preservative system can trigger a recall.
In 2022, 62.7% of stability professionals surveyed by the Parenteral Drug Association reported a product recall in the past five years. The top reason? Microbial growth due to changes in water activity - often caused by poor packaging or storage.

What’s Changing in 2025?
The rules are evolving. The ICH Q12 guideline, effective since late 2023, allows manufacturers to make post-approval changes to packaging or processes without restarting full stability studies - as long as they can prove it won’t affect safety. This is a big shift. It means faster innovation, but also more responsibility on companies to monitor their products after launch.Another trend? Predictive modeling. Companies like Amgen and Merck are using risk-based tools to predict degradation patterns without waiting years. In pilot studies, they cut shelf-life determination time by 30%. But regulators are still cautious. Just because a model predicts stability doesn’t mean it’s accepted. The FDA still wants real data.
Climate change is adding pressure. A 2022 MIT study found that rising global temperatures could reduce average drug shelf life by nearly five months by 2050. Warehouses in major distribution hubs are already hitting 30°C for over 87 days a year. That’s beyond the “room temperature” range. What happens to your medicine in a truck in Texas in July? Or a warehouse in Mumbai in June?
What Should You Do?
You can’t control how your medicine is stored before you buy it. But you can control what happens after.- Check expiration dates. Don’t use anything past its date - even if it looks fine.
- Store medicines in a cool, dry place. Not the bathroom. Not the kitchen window. A closet shelf away from heat and humidity is best.
- Don’t transfer pills to pill organizers unless they’re designed for long-term use. Some plastics absorb moisture and accelerate degradation.
- If you’re using a generic, and you notice a change in how it works - less effective, new side effects - talk to your pharmacist. It might not be you. It might be the drug.
- For food, check for off smells, colors, or textures. If it looks or smells wrong, throw it out. No one needs botulism.
Stability testing isn’t glamorous. It doesn’t make headlines. But it’s the invisible guardrail between you and harm. Every time you take a pill, you’re trusting that someone did the work to make sure it wouldn’t hurt you. Don’t take that trust for granted.
Can I still use medicine after its expiration date?
The FDA says no. While some drugs may remain chemically stable past their expiration date, there’s no guarantee of safety or effectiveness. Degradation can happen unpredictably - especially with liquids, suspensions, or insulin. Using expired medication risks underdosing, overdosing, or exposure to toxic breakdown products. Always dispose of expired drugs properly.
Why do generic drugs sometimes have different shelf lives than brand-name ones?
Generics must match the brand in active ingredient and absorption, but not necessarily in excipients or packaging. Different fillers, coatings, or moisture barriers can affect how quickly the drug degrades. A generic with a thinner capsule or less effective seal might have a shorter shelf life - even if the active ingredient is identical. Always check the label for the expiration date specific to the product you’re holding.
Does refrigerating medicine always make it last longer?
Not always. Some medications are designed to be stable at room temperature. Refrigeration can cause condensation inside the container, leading to moisture damage - which speeds up degradation. Always follow the storage instructions on the label. If it says "store at room temperature," don’t put it in the fridge unless your pharmacist says it’s safe.
How do I know if my generic drug is unstable?
Signs include: pills that crumble easily, capsules that stick together, liquids that change color or become cloudy, or tablets with an odd smell (like vinegar). If you notice any change in how the medicine works - like your blood pressure not dropping or your asthma inhaler not helping - talk to your pharmacist. Report it. These changes are often early warnings of instability.
Are there any drugs that are more prone to degradation?
Yes. Liquid medications, insulin, nitroglycerin, certain antibiotics like tetracycline, and some psychiatric drugs (like lithium) are especially sensitive to heat, light, and moisture. Nanoparticle-based drugs and those with complex delivery systems (like inhalers or patches) also degrade more easily. Always check the product’s stability profile - your pharmacist can help.





Emmanuel Peter
December 4, 2025 AT 17:26Ashley Elliott
December 5, 2025 AT 07:18Chad Handy
December 7, 2025 AT 00:11Chase Brittingham
December 7, 2025 AT 15:36Bill Wolfe
December 9, 2025 AT 01:31Benjamin Sedler
December 9, 2025 AT 09:04zac grant
December 10, 2025 AT 03:46Gareth Storer
December 11, 2025 AT 07:25Pavan Kankala
December 12, 2025 AT 15:36Martyn Stuart
December 12, 2025 AT 21:18Yasmine Hajar
December 14, 2025 AT 03:15Karl Barrett
December 15, 2025 AT 02:43Jake Deeds
December 15, 2025 AT 09:30John Filby
December 16, 2025 AT 18:45Ben Choy
December 17, 2025 AT 21:26