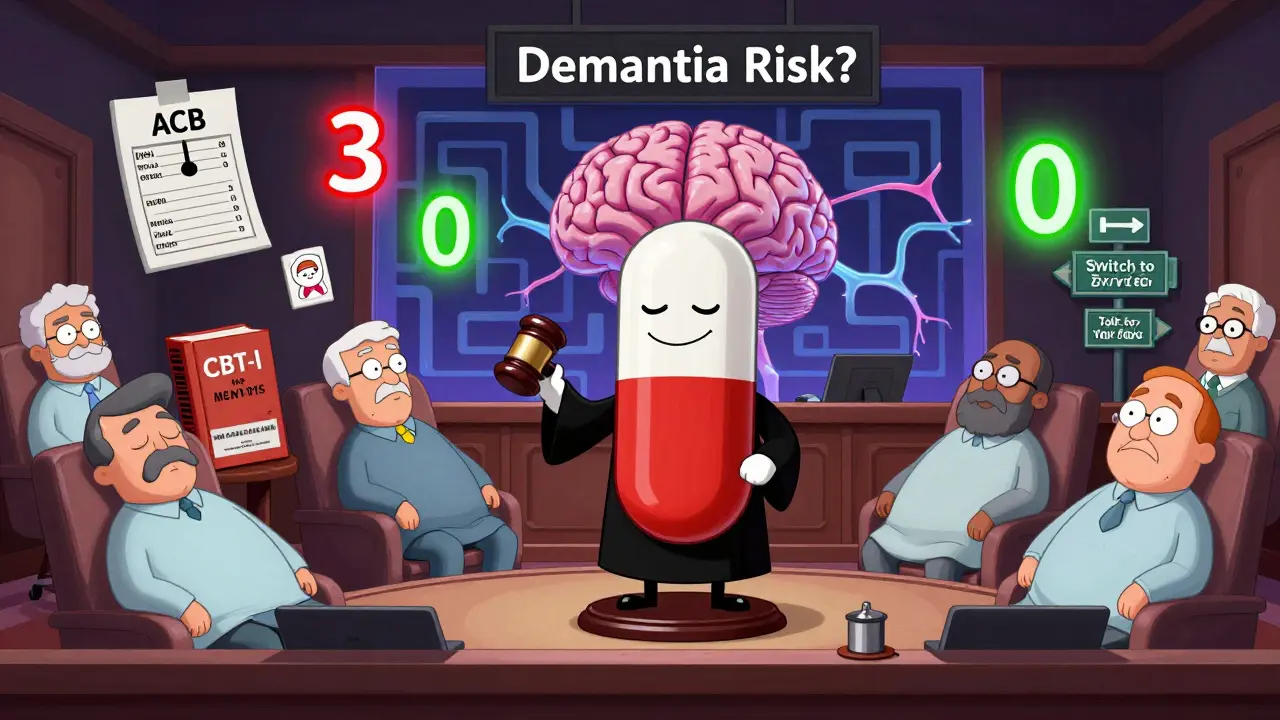
Anticholinergic Burden Calculator
Medication Review Tool
Enter medications you're currently taking to calculate your total anticholinergic burden score. This score helps identify potential cognitive risks associated with your medication regimen.
Current Medications
Results
Total Anticholinergic Burden Score
0Risk Level:
Recommendations
The Anticholinergic Cognitive Burden (ACB) scale measures the potential cognitive effects of medications. Scores range from 0 (no anticholinergic activity) to 3 (strong anticholinergic activity). Higher scores may increase risk of cognitive decline and dementia.
Many older adults in the UK and beyond reach for over-the-counter antihistamines like Benadryl to help them sleep or manage allergies. It’s easy to think of these pills as harmless - they’ve been around for decades, sold on every pharmacy shelf, and promoted as quick fixes. But what if taking them every night for years could quietly increase your risk of memory problems? The science isn’t simple, but the warning signs are real.
Not All Antihistamines Are the Same
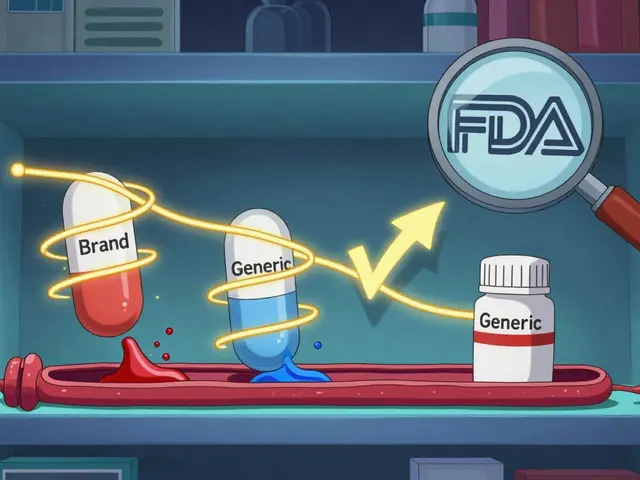
There are two main types of antihistamines: first-generation and second-generation. The difference isn’t just in brand names - it’s in how they affect your brain.First-generation antihistamines like diphenhydramine (Benadryl), doxylamine (Unisom), and chlorpheniramine cross the blood-brain barrier. Once inside, they block acetylcholine, a chemical your brain needs to form memories and stay alert. This is why they make you drowsy - and why they’ve been linked to cognitive decline over time.
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were designed to avoid this. They don’t cross into the brain as easily. They’re just as good for allergies, but they don’t mess with your memory the same way. Studies show their anticholinergic effect is 100 to 1,000 times weaker than first-gen versions.
The Dementia Connection: What the Studies Say
A major 2015 study in JAMA Internal Medicine followed over 3,400 people over age 65 for 10 years. It found that long-term use of strong anticholinergic drugs - including some antihistamines - was tied to higher dementia risk. But here’s the twist: when researchers looked only at antihistamines, the link vanished. Other drugs like certain antidepressants and bladder medications showed clear risks, but antihistamines didn’t.Another study in 2022, looking at nearly 9,000 older adults, found that people taking first-gen antihistamines had higher dementia rates - 3.8% compared to 1% in those using second-gen. But when they adjusted for other factors like age, health conditions, and sleep problems, the difference wasn’t statistically significant. That means the numbers could be due to chance.
Even more confusing? A 2021 meta-analysis that grouped all anticholinergics together found a 46% higher dementia risk. But when you pull antihistamines out of that mix, the risk drops to near zero. This suggests the real danger might come from other types of drugs - not antihistamines alone.
Why the Confusion? It’s Not Just the Drug
Many people who take diphenhydramine nightly do so because they have insomnia. And insomnia itself is linked to dementia. So when studies see a connection between antihistamine use and memory loss, are they seeing the drug’s effect - or the effect of poor sleep?A 2023 analysis from the UK Biobank found that when researchers controlled for sleep disorders, the link between antihistamines and dementia disappeared. That’s a big clue. It suggests the problem isn’t necessarily the pill - it’s the reason people are taking it.
Also, older adults often take multiple medications. One anticholinergic pill might not hurt. But if you’re on three or four - a bladder drug, a sleep aid, an antidepressant - the effects add up. That’s why the American Geriatrics Society warns against stacking anticholinergics. It’s the cumulative burden that matters.

What Experts Are Saying
Dr. Shelley Gray, who led the landmark 2015 study, says: “The association appears strongest for specific drug classes like antidepressants and bladder medications, not uniformly across all anticholinergics.” She doesn’t see antihistamines as the main culprit.But Dr. Malaz Boustani, a leading expert on cognitive aging, takes a different view. He warns that even small doses can pile up over time, especially in people with diabetes, heart disease, or other chronic conditions. “Your brain doesn’t recover as easily after 65,” he says. “Every anticholinergic drug adds a little strain.”
The American Geriatrics Society’s 2023 Beers Criteria gives first-gen antihistamines a clear “Avoid” rating for people over 65. That’s Level A evidence - the strongest possible. The European Medicines Agency, meanwhile, says the evidence is inconsistent - but still recommends warning labels on packaging.
Real People, Real Choices
On Reddit, a geriatric care manager with over 2,000 karma wrote: “83% of my clients over 70 were taking diphenhydramine nightly for sleep, completely unaware of potential long-term risks.” That’s not an outlier. A 2022 survey by the National Council on Aging found that 42% of older adults regularly used OTC antihistamines for sleep. And 78% had no idea they were anticholinergic.One user on AgingCare.com shared: “My mother’s doctor prescribed Benadryl for years to help her sleep, and now she has dementia - I can’t help but wonder if there’s a connection.” Her story isn’t rare. But it’s also not proof.
The truth is messy. We don’t have a smoking gun. But we do have enough red flags to pause and rethink.
What Should You Do Instead?
If you or someone you love is taking diphenhydramine for sleep, here’s what to consider:- Switch to a second-gen antihistamine. Loratadine, cetirizine, or fexofenadine work just as well for allergies - and don’t affect your brain.
- Try non-drug sleep solutions. Cognitive Behavioral Therapy for Insomnia (CBT-I) works for 70-80% of older adults. It’s not magic, but it’s proven. The problem? Waitlists are long - often over 8 weeks - and Medicare only covers about $100 per session.
- Check your meds. Use the Anticholinergic Cognitive Burden Scale (ACB). Diphenhydramine scores a 3 - the highest risk. Fexofenadine? A 0. Ask your pharmacist to review all your pills at least once a year.
- Don’t stop cold turkey. Suddenly quitting can cause rebound insomnia or worse. Talk to your doctor first.
The Choosing Wisely campaign, backed by the American Board of Internal Medicine, specifically says: “Avoid diphenhydramine for chronic insomnia in older adults.” That’s not a suggestion - it’s a guideline.
What’s Changing Now?
The market is shifting. First-gen antihistamine sales dropped 24% between 2015 and 2022. Second-gen sales rose 18%. More pharmacies now put warning stickers on diphenhydramine bottles. The FDA is reviewing all anticholinergics - final results expected in mid-2024.Pharmaceutical companies are responding too. Low-dose doxepin (Silenor), approved for insomnia in 2010, has minimal anticholinergic effects and now holds 12% of the prescription sleep aid market. It’s not cheap, but it’s safer.
And the American Geriatrics Society is preparing its 2024 Beers Criteria update. It’s expected to give more precise, drug-by-drug guidance - not just blanket warnings.
Bottom Line: Be Smart, Not Scared
You don’t need to panic if you’ve taken Benadryl for years. But you do need to act now.If you’re using first-gen antihistamines for sleep or allergies, talk to your doctor. Ask: “Is there a safer alternative?” Switching to loratadine or cetirizine is easy. It’s not a miracle cure, but it removes one potential risk factor from your daily routine.
And if you’re worried about memory changes, don’t blame the pill alone. Look at your whole picture: sleep, stress, other meds, activity levels. Dementia isn’t caused by one drug. It’s shaped by years of small choices - and one of them might be what’s on your nightstand.
Knowledge is power. And right now, the safest thing you can do is stop assuming that “over-the-counter” means “safe forever.”





Kelly McRainey Moore
January 21, 2026 AT 00:30Been using Zyrtec for years instead of Benadryl-never even knew there was a difference until now. My grandma took diphenhydramine like candy, and I always thought it was just ‘her thing.’ Now I’m checking her meds list. Thanks for this.
michelle Brownsea
January 22, 2026 AT 05:09Let’s be real: if you’re popping Benadryl like it’s candy, you’re not just risking dementia-you’re surrendering your brain to corporate pharmacy marketing. These pills were never meant for nightly use! The FDA’s been warning about anticholinergics since 2012, and yet? People still think ‘over-the-counter’ means ‘safe forever.’ It’s not ignorance-it’s willful neglect. Wake up. Your hippocampus isn’t a vending machine.
Roisin Kelly
January 23, 2026 AT 02:41They’re lying. This is all a Big Pharma scam to sell you expensive ‘second-gen’ drugs. Diphenhydramine’s been around since 1946-how many wars did soldiers take it in? They didn’t all get dementia. The real cause? 5G brain rot. And glyphosate. And the moon. You think they want you to know the truth? Nah.
lokesh prasanth
January 25, 2026 AT 02:13Anticholinergic load > single drug. Sleep problem = root cause. Drug is symptom. Fix sleep, not pill. Simple.
Ashok Sakra
January 25, 2026 AT 10:50My aunt took Benadryl for 17 years and now she doesn’t recognize me. I saw it happen. Slow. Silent. Like a ghost stealing her mind. And the doctor? He just nodded and wrote another script. This isn’t science-it’s betrayal.
Andrew Rinaldi
January 27, 2026 AT 01:07I think the real takeaway here is nuance. Some people are at risk. Others aren’t. It’s not about fear-it’s about awareness. If you’re on three or more anticholinergics, it’s worth a pharmacist review. If you’re on one for allergies? Probably fine. Context matters.
Gerard Jordan
January 28, 2026 AT 07:08Just switched my dad to loratadine last week. He thought it wouldn’t work, but he’s sleeping just as well-no zombie mode anymore 😊 Also told him to try melatonin. He’s still skeptical, but he’s trying. Small wins, right?
Yuri Hyuga
January 28, 2026 AT 16:19As a geriatric nurse in London, I’ve seen this pattern for decades. The most heartbreaking part? Patients never connect the dots until it’s too late. We need better labeling, yes-but we also need public health campaigns. Not just for seniors, but for their families. Knowledge is the first step. Thank you for this post-it’s a lifeline.
Coral Bosley
January 28, 2026 AT 17:06Benadryl is the poor man’s Valium. And if you’re using it to sleep, you’re probably also drinking too much wine, scrolling until 2 a.m., and eating three bags of chips a day. The pill isn’t the villain-it’s the scapegoat for a whole lifestyle that’s falling apart.
MAHENDRA MEGHWAL
January 29, 2026 AT 08:30Respectfully, the evidence remains inconclusive. While observational studies suggest an association, causation has not been established. The confounding variables-including pre-existing cognitive decline leading to self-medication-are significant. A prudent approach would be to avoid unnecessary polypharmacy, but not to vilify a widely used and historically benign agent without definitive longitudinal data.
Sangeeta Isaac
January 29, 2026 AT 10:15So… I’ve been taking Benadryl for allergies since 2010 and I still think my cat is plotting to steal my socks. Maybe it’s the drug? Or maybe she’s just a little psycho 😏 Anyway, gonna switch to Zyrtec. If I start remembering where I put my keys, I’ll send you a thank-you card.