When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck. It’s the result of strict CGMP rules enforced by the FDA. These aren’t suggestions-they’re legal requirements that every generic drug manufacturer must follow, no matter where they’re based. If they don’t, the product gets pulled, the factory gets shut down, or worse, people get hurt.
What Exactly Is CGMP?
CGMP stands for Current Good Manufacturing Practices. The "current" part is critical. It means manufacturers can’t just follow old methods-they have to use up-to-date technology, systems, and controls. The FDA doesn’t just want you to avoid mistakes; it wants you to build systems that prevent them from ever happening. These rules are written into federal law under 21 CFR Parts 210 and 211. They cover everything from how a factory is built to how records are kept. And yes-generic drugs must meet the exact same standards as brand-name drugs. There’s no "light version" of quality for generics. Pfizer, Teva, and smaller manufacturers all play by the same playbook.Who Makes Sure These Rules Are Followed?
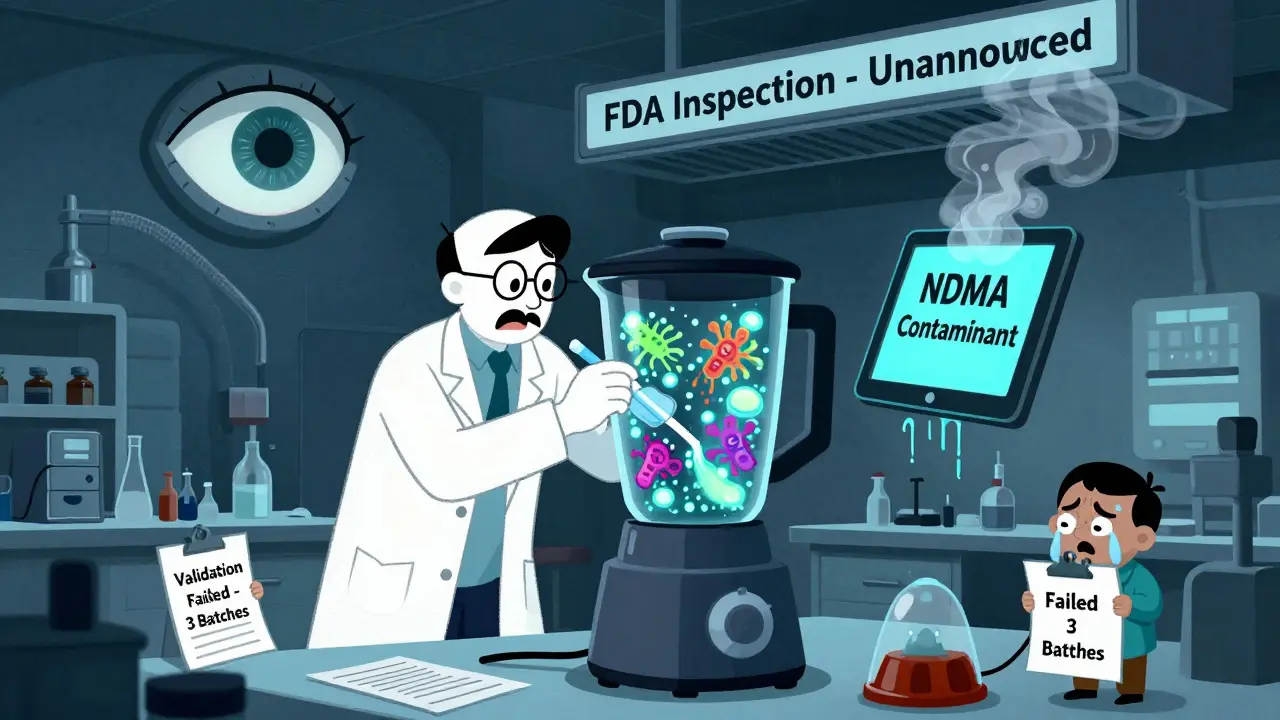
The FDA’s Office of Compliance does the checking. Inspectors show up unannounced at manufacturing sites-domestic and foreign-and dig into every detail. They look at training logs, equipment calibration records, lab test results, and even how workers clean machines between batches. In 2022, FDA inspectors issued over 400 Warning Letters related to CGMP violations. Nearly two-thirds of those went to foreign facilities, mostly in India and China. But that doesn’t mean U.S. plants are clean. Labs and production areas are the most common trouble spots. One 2022 report found that 41% of all violations were tied to laboratory controls and production process controls. The penalty for failing? The drug becomes "adulterated" under the law. That means it can’t be sold. Companies can face fines, import bans, or even criminal charges.The 11 Key Areas of CGMP Compliance
The rules are broken into 11 subparts. Here’s what they actually mean in practice:- Organization and Personnel (§211.25): Everyone who touches the product needs documented training. Not just a one-time class-annual refreshers. The Quality Unit has to be independent and powerful enough to stop production if something’s wrong.
- Buildings and Facilities (§211.46): Air filters, humidity controls, separate areas for different processes. Dust and moisture can ruin a batch. A clean room isn’t optional.
- Equipment (§211.68): Every machine must be calibrated. Every cleaning procedure must be tested. If a blender isn’t cleaned properly between batches, cross-contamination can happen. Swab tests must show no more than 100 colony-forming units (CFU) per surface.
- Control of Components (§211.84): Every ingredient, even something as simple as lactose, must be tested before use. In 2022, 43% of generic manufacturers had at least one component fail testing.
- Production and Process Controls (§211.100-113): You can’t just wing it. Every step-mixing, granulating, compressing-must be validated. That means proving, with data, that your process consistently makes the same product. Most companies use three consecutive batches for validation.
- Packaging and Labeling (§211.122): Labels must be verified before they go on the bottle. A wrong label means a wrong dose. That’s a recall waiting to happen.
- Holding and Distribution (§211.142): Temperature matters. If your drug needs to stay cool, you must prove it stayed cool during transport and storage.
- Laboratory Controls (§211.166): Stability testing isn’t optional. You have to prove the drug won’t break down over time. That means storing samples for months or years and testing them periodically.
- Records and Reports (§211.180): You must keep every record for at least one year after the drug expires. Electronic records? They must follow Part 11 rules-audit trails, secure logins, no backdating.
- Returned and Salvaged Products (§211.210): If a customer sends back a bottle, it can’t just be thrown back on the shelf. It must be quarantined and evaluated.
Why Do Some Companies Struggle?
Small generic manufacturers often get crushed under the weight of these rules. A 2022 survey found that 68% of mid-sized firms had trouble just keeping up with documentation. One company on Reddit said switching to electronic batch records cost $1.2 million and took 14 months. Compliance costs average $2.3 million per year for a mid-sized generic maker. That’s not profit-it’s survival. And it’s why big companies like Teva have 97% compliance rates, while smaller ones hover around 82%. The biggest pain points? Data integrity and supply chain control. Many manufacturers can’t properly track who changed what in their systems. And when your active ingredient comes from a supplier in another country, you’re one bad batch away from a nationwide recall.Recent Changes and Future Trends
In May 2023, the FDA issued an immediate guidance requiring testing for toxic contaminants like diethylene glycol in high-risk ingredients like glycerin. This came after deaths in Pakistan linked to contaminated cough syrup. It’s a reminder: CGMP isn’t about paperwork-it’s about preventing tragedy. The FDA’s 2023-2027 plan includes more inspections of foreign plants and a push for advanced manufacturing. Continuous manufacturing-where drugs are made in one long, uninterrupted flow instead of in batches-is the future. But it’s hard to validate under old CGMP rules. The FDA is working on new guidance expected in 2024. Industry experts predict that by 2028, 65% of manufacturers will use AI and predictive analytics to catch quality issues before they happen. That’s the next level: not just checking after the fact, but stopping problems before they start.
What Happens When CGMP Fails?
The 2022 recall of 12 generic metformin products is a textbook case. The FDA found that cleaning procedures weren’t validated, and contamination from a previous batch got into new ones. The contaminant? NDMA, a probable carcinogen. The result? Millions of pills pulled, lawsuits filed, and trust shaken. Another failure? When a lab falsifies test results. That’s not a mistake-it’s fraud. And the FDA treats it that way. In 2022, 63% of data integrity warning letters targeted foreign facilities where oversight is harder.How to Stay Compliant
If you’re building or running a generic drug facility, here’s what works:- Start with a solid Quality Management System (QMS). Document everything-even the obvious stuff.
- Train your team constantly. The FDA checks training logs. If it’s not written down, it didn’t happen.
- Invest in electronic systems. Paper records are a liability. eQMS platforms reduce audit findings by 40%.
- Validate every process. Don’t assume it works-prove it.
- Test your suppliers. Don’t trust their certificates. Do your own checks.
- Prepare for inspections. Know every procedure inside out. Inspectors will ask you to show it live.
Final Reality Check
CGMP isn’t about perfection. It’s about control. It’s about knowing that every pill you make is safe, effective, and consistent. The FDA doesn’t care if you’re big or small. They don’t care if you’re in Ohio or Odisha. If you’re selling a generic drug in the U.S., you follow the same rules as Pfizer. The system isn’t perfect. There are inconsistencies in inspections. Costs are high. But the result? 90% of prescriptions filled in the U.S. are generics-and almost all of them work exactly as they should. That’s not magic. That’s CGMP.Are generic drugs held to the same quality standards as brand-name drugs?
Yes. The FDA requires that generic drugs meet the exact same Current Good Manufacturing Practices (CGMP) as brand-name drugs. This includes identical standards for facility design, equipment, testing, documentation, and process validation. The FDA does not allow lower standards for generics, and every manufacturing site-whether domestic or foreign-is subject to the same inspection protocols.
What happens if a generic drug manufacturer violates CGMP rules?
Violations can lead to warning letters, import alerts, product recalls, or even a complete shutdown of production. The FDA can legally declare the product "adulterated," making it illegal to sell. In severe cases, including fraud or falsified data, companies face civil penalties or criminal charges. Foreign manufacturers may be barred from importing into the U.S. entirely.
How often does the FDA inspect generic drug facilities?
Domestic facilities are inspected on average every 18 months, while foreign facilities are inspected less frequently-though the FDA is increasing foreign inspection rates. High-risk facilities, those with past violations, or those producing complex drugs may be inspected more often. The FDA uses risk-based scheduling, meaning some sites get checked annually, while others may wait longer if they have strong compliance histories.
What is the biggest challenge for small generic manufacturers under CGMP?
The biggest challenge is cost and complexity of compliance, especially around documentation and electronic records. Small firms often lack the staff or budget to implement full electronic quality management systems (eQMS), maintain audit trails, or validate complex processes. Many report spending over $2 million annually just to meet CGMP requirements, which can make it hard to compete with larger companies.
Why does the FDA focus so much on data integrity?
Data integrity is the foundation of trust. If test results, batch records, or equipment logs can be altered or deleted, there’s no way to know if the drug is safe or effective. The FDA’s ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available) are used to ensure records are reliable. Over 78% of manufacturers report difficulty meeting Part 11 requirements for electronic records, making this the most common violation area.
Are CGMP rules changing for new manufacturing technologies like continuous manufacturing?
Yes. Traditional CGMP was built around batch manufacturing, but continuous manufacturing-where drug production runs nonstop-is becoming more common. The FDA is updating its guidance to accommodate this shift, focusing on real-time monitoring and process analytics instead of just end-product testing. Draft guidance for continuous manufacturing is expected in 2024, and companies using these technologies are already working with the FDA’s Emerging Technology Program.
Can a generic drug be approved without full CGMP compliance?
No. CGMP compliance is mandatory for approval of any generic drug. The FDA reviews manufacturing practices as part of every Abbreviated New Drug Application (ANDA). If the inspection finds major violations, the application is refused. Even if the drug formula is identical to the brand, without proven CGMP compliance, it cannot be legally sold in the U.S.







Mark Able
December 17, 2025 AT 20:01Man, I just got my generic blood pressure med last week and I was thinking about this exact thing. Like, how the hell do they make sure it’s not just sugar pills with fancy packaging? The FDA’s got this locked down tighter than my ex’s Instagram account. No way they’d let some sketchy factory in Delhi ship out crap that could kill someone. I mean, I trust my doctor, but I don’t trust the system-until I read stuff like this. Then I’m like, okay, maybe they’re not all corrupt.
James Stearns
December 18, 2025 AT 10:19It is of paramount importance to underscore that Current Good Manufacturing Practices, as codified under Title 21 of the Code of Federal Regulations, constitute a non-negotiable statutory imperative-not a recommendation, not a guideline, not a suggestion. The FDA’s enforcement apparatus, though under-resourced, remains the sole bulwark against systemic pharmaceutical degradation. To suggest otherwise is to invite public health catastrophe.
Nina Stacey
December 19, 2025 AT 02:27Wow I never realized how much goes into making a simple pill like this like I just thought it was like baking cookies but way more sterile and I’m so impressed by how much work they do to make sure we’re not getting poisoned like the cleaning tests and the humidity control and the training and honestly I feel way better about my meds now even though I used to be super suspicious about generics cause they’re cheaper but now I get it they’re not cheap because they’re bad they’re cheap because they don’t have to spend millions on ads
Kinnaird Lynsey
December 19, 2025 AT 05:43Interesting how the same rules apply whether you're in Ohio or Odisha. Makes you wonder why we treat foreign facilities like suspects and domestic ones like saints. The data shows violations are everywhere. Maybe the real issue isn’t location-it’s that we expect perfection from a system that’s always underfunded and overworked.
Andrew Kelly
December 20, 2025 AT 17:54Let me guess-this is all just a corporate scam to keep prices high. The FDA is in bed with Big Pharma. They let Pfizer get away with everything, but now they’re cracking down on generics to scare people into buying the $200 brand-name version. That’s why they focus on foreign labs-distraction tactic. Meanwhile, the real problem? Drug companies lobbying to weaken oversight. You think they care about safety? They care about profit margins.
Moses Odumbe
December 21, 2025 AT 01:01Bro. This is wild. 🤯 I didn’t know they swab machines for bacteria. Like… 100 CFU? That’s less than a poppy seed’s worth of gunk. And they keep records for a YEAR after expiration? Who even does that? 🧠 I’m impressed. Also, AI in pharma? That’s next level. 🤖💊
Vicki Belcher
December 22, 2025 AT 08:25It’s kinda beautiful how something so technical-calibration logs, audit trails, stability testing-ends up being what keeps you alive. I take my meds every day without thinking. But this? This is the quiet hero work. No parades. No headlines. Just people in lab coats making sure your pill doesn’t turn into poison. 🙏
anthony funes gomez
December 23, 2025 AT 15:31CGMP-Current Good Manufacturing Practices-exists as a dialectical counterpoint to the ontological instability of pharmaceutical production: the very notion that a molecule, identical in composition, may vary in efficacy due to procedural entropy. The FDA’s insistence on validation is not regulatory overreach-it is epistemological necessity. Without documented, reproducible, and traceable process control, identity becomes indeterminate. The pill ceases to be a pharmacological entity-it becomes an accident.
William Liu
December 25, 2025 AT 09:13One of the few things in healthcare that actually works the way it’s supposed to. No hype. No fluff. Just rules, inspections, and accountability. That’s why generics work. Not because they’re cheap-but because they’re held to the same standard as the expensive stuff. We should be proud of this system.
Glen Arreglo
December 26, 2025 AT 04:43India and China get blamed a lot, but let’s be real-this is a global system. I’ve worked in pharma labs in three countries. The people doing the work? They’re not criminals. They’re overworked, underpaid, and stuck with outdated equipment because their company cut corners to stay competitive. The real villain isn’t the factory-it’s the pricing model that forces everyone to race to the bottom. Fix that, and compliance improves on its own.
shivam seo
December 26, 2025 AT 22:21So you’re telling me the FDA spends millions checking if a pill’s clean… while our roads are falling apart and schools are crumbling? This is why America’s broken. Priorities. We’re obsessed with regulating pills but ignore real problems. You think a $2 generic is safe? Maybe. But you think your kid’s school has lead-free water? Nah.