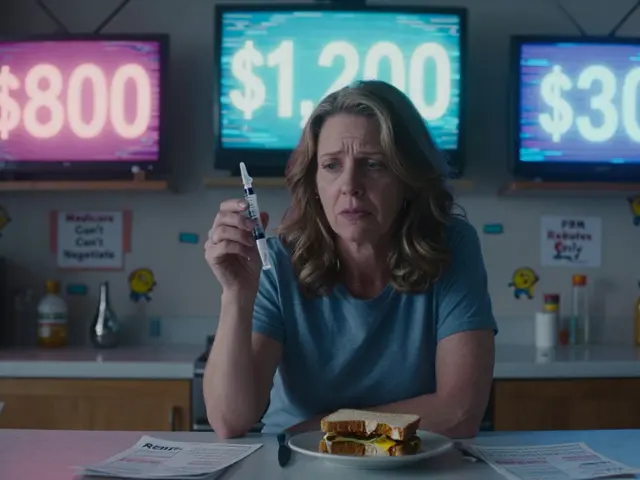
Every year, millions of Americans face a brutal choice: pay for their medicine or pay for rent. It’s not a hypothetical. It’s real. A woman in Ohio skips her insulin doses every other day to make it last. A veteran in Texas buys his heart medication from Canada because his local pharmacy charges $700 a month. And yet, the same pills cost $30 in Germany and $45 in the UK. Why does this happen? Why are prescription drugs so expensive in the United States?
The System Was Built to Let Companies Charge Whatever They Want
Unlike every other wealthy country, the U.S. doesn’t let the government negotiate drug prices for Medicare - the program that covers over 65 million people. Back in 2003, Congress passed the Medicare Modernization Act and made it illegal for Medicare to bargain for lower prices. That decision created a power imbalance that still exists today. Drugmakers know they can set any price they want, and Medicare has to pay it. No other developed nation allows this. Canada, the UK, France, and Germany all negotiate directly with manufacturers. The U.S. doesn’t. That’s not an accident. It was designed this way.Pharmaceutical Companies Make Most of Their Profits in the U.S.
The U.S. has less than 5% of the world’s population. But it accounts for nearly 75% of all global pharmaceutical profits. That’s not because Americans are sicker. It’s because they pay more. The same exact pill, made in the same factory, sold to the same patient, costs over three times more in the U.S. than in other rich countries. Take Galzin, a drug for Wilson’s disease. In the U.S., it costs $88,800 a year. In the UK, it’s $1,400. In Germany, $2,800. That’s not a pricing error. That’s business strategy. Companies know the U.S. market has no price controls, so they charge what the market will bear - and the market has no leverage.Pharmacy Benefit Managers (PBMs) Make It Worse
You’ve probably never heard of PBMs, but they’re one of the biggest reasons drug prices keep climbing. These companies were supposed to help negotiate discounts for insurers. Instead, they’ve become powerful middlemen with their own profits tied to high list prices. PBMs get paid based on rebates - the discounts drugmakers offer them after setting a high sticker price. So the higher the price, the bigger the rebate. The bigger the rebate, the more money the PBM makes. That’s why a drug might be listed at $1,000, even though the real cost to make it is $5. The PBM takes a cut, the insurer takes a cut, and the patient still pays the full list price at the pharmacy counter. It’s a rigged game.
The Inflation Reduction Act Tried to Fix It - But It’s Not Enough
In 2022, Congress passed the Inflation Reduction Act. For the first time, Medicare could negotiate prices for a small number of drugs. In 2026, that list includes ten drugs - mostly for diabetes, heart failure, and immune disorders. That’s a start. But it’s not a solution. The law only applies to Medicare Part D, which covers seniors. It doesn’t touch private insurance. And even for Medicare, the number of drugs eligible for negotiation is tiny. In 2025, the law also forced drugmakers to pay rebates if they raised prices faster than inflation. That saved money on 64 drugs. But in 2024, overall drug spending jumped 11.4% - up from 4.9% the year before. That growth was driven by new, expensive drugs for obesity and diabetes. Those drugs? They’re still priced at $1,000 a month. And they’re selling like crazy.Specialty Drugs Are Breaking the System
The biggest cost drivers today aren’t old pills. They’re new, complex drugs - called specialty drugs - for cancer, rare diseases, and metabolic conditions. These drugs cost $100,000 or more a year. They’re made by a handful of companies with little competition. One drug for a rare liver disease costs $300,000 a year in the U.S. In Switzerland, it’s $40,000. Why? Because there’s no one to push back. These drugs often have patents that block generics for decades. And even when generics exist, PBMs and insurers often don’t push them because the rebates on brand-name drugs are too lucrative. The result? Patients pay more. Hospitals pay more. Taxpayers pay more. And drugmakers make billions.Politicians Promise Change - But Prices Keep Rising
You’ve heard the promises. “We’re going to lower drug prices.” “Americans shouldn’t pay more than other countries.” But here’s the truth: since 2020, over 688 prescription drugs have gone up in price - even as presidents and senators made speeches about lowering them. In 2025, Senator Bernie Sanders found that 87 drugs got more expensive after President Trump sent letters to drug companies asking them to lower prices. Meanwhile, the White House announced five new deals - lowering Ozempic from $1,000 to $350 a month, Wegovy from $1,350 to $350. Sounds good, right? But those are voluntary deals. They’re not laws. The next company can still charge $1,500 for the same drug. And most drugs aren’t part of these deals. Only a fraction. The system is still broken.
What Happens When Patients Can’t Pay?
One in four Americans says they’ve skipped a dose, cut a pill in half, or gone without medicine because they couldn’t afford it. For Medicare beneficiaries, the new $2,000 out-of-pocket cap helps - but only if they’re on Medicare Part D. Many seniors still pay thousands a year. And if Project 2025’s proposed plan passes, that cap could disappear for millions. Imagine being 72, diabetic, and choosing between insulin and your heating bill. That’s not a policy debate. That’s a human crisis. And it’s happening every day.The Real Problem? No One Has the Power to Say No
In other countries, the government says: “This drug costs too much. We won’t cover it unless you lower the price.” In the U.S., no one says no. Insurers can’t. Medicare can’t. Patients can’t. Even when a drug is proven to be overpriced, there’s no mechanism to force change. The drugmaker holds all the cards. And until Congress gives Medicare real negotiation power - not just for 10 drugs, but for hundreds - prices will keep rising. Until PBMs are forced to pass savings to patients, not pocket rebates, patients will keep paying more. Until patents are reined in and competition is allowed, the same companies will keep charging the same insane prices.The U.S. doesn’t have a drug pricing crisis. It has a policy failure. The system was designed to benefit drugmakers, not patients. And until that design changes, nothing will.
Why do U.S. drug prices cost more than in other countries?
The U.S. is the only developed country that doesn’t let its government negotiate drug prices for Medicare. Other nations use reference pricing, bulk buying, or direct talks to keep costs down. In the U.S., drugmakers set prices freely, and no one can legally force them to lower them. This system lets companies charge up to three times more than in Europe or Canada for the same drug.
What role do Pharmacy Benefit Managers (PBMs) play in high drug prices?
PBMs were created to negotiate discounts for insurers, but now they often profit from high list prices. They receive rebates from drugmakers based on how high the sticker price is - not how low the final cost is. So they have an incentive to keep prices high, even if patients pay more out of pocket. This hidden rebate system adds layers of cost that aren’t transparent to consumers.
Has the Inflation Reduction Act lowered drug prices?
Yes, but only for a few drugs. Starting in 2026, Medicare can negotiate prices for 10 drugs - mostly for chronic conditions. It also forced companies to pay rebates if they raised prices faster than inflation. So far, 64 drugs have seen lower costs for Medicare beneficiaries. But these changes cover less than 1% of all prescription drugs. For most people, prices are still rising.
Why are specialty drugs so expensive?
Specialty drugs - like those for cancer, diabetes, and rare diseases - are complex to make and often have little competition. Drugmakers hold long-term patents and charge high prices because there’s no alternative. Many cost over $100,000 a year. Even when generics exist, PBMs and insurers often don’t promote them because the rebates on brand-name versions are more profitable.
Can Americans buy cheaper drugs from other countries?
Technically, yes - but it’s not legal for individuals to import most prescription drugs from Canada or Mexico. Some people do it anyway, especially for insulin or heart meds. The FDA doesn’t actively stop it, but there’s no guarantee the drugs are safe or properly labeled. A few states have started official import programs, but they’re small-scale and don’t solve the broader problem.
Will the proposed Project 2025 plan make drug prices worse?
Yes, according to the Center for American Progress. Their analysis shows Project 2025’s plan would eliminate or weaken current cost protections, including the Medicare out-of-pocket cap. As many as 18.5 million seniors and people with disabilities could face higher drug costs under that plan. It would also remove limits on how much PBMs can charge and reduce oversight of drug pricing.
Why haven’t lawmakers fixed this yet?
The pharmaceutical industry spends over $300 million a year lobbying Congress. That’s more than any other industry. Lawmakers who support drug price reform often face pressure from donors, campaign contributions, and threats of funding cuts. Even when public opinion is strong, the money and influence behind the status quo are too powerful to overcome quickly.





clarissa sulio
February 3, 2026 AT 00:52Bridget Molokomme
February 4, 2026 AT 19:50jay patel
February 6, 2026 AT 04:37Ansley Mayson
February 6, 2026 AT 07:28phara don
February 7, 2026 AT 20:45Hannah Gliane
February 8, 2026 AT 03:15Murarikar Satishwar
February 8, 2026 AT 15:18Dan Pearson
February 9, 2026 AT 01:29Eli Kiseop
February 10, 2026 AT 02:09Gary Mitts
February 12, 2026 AT 02:09Vatsal Srivastava
February 13, 2026 AT 07:50Brittany Marioni
February 15, 2026 AT 06:49Monica Slypig
February 15, 2026 AT 07:23Becky M.
February 15, 2026 AT 23:49Bob Hynes
February 17, 2026 AT 19:12