TCA Side Effect Predictor
How This Tool Works
Enter your TCA medication type and dose to see the most common side effects based on clinical evidence. This tool uses data from the article to predict side effects, but always consult with your doctor about medication risks.
Predicted Side Effects
- Dry mouth (common)
- Drowsiness (common)
- Blurred vision
- Constipation
- Urinary retention
- Dizziness
- Fast heartbeat
Note: This prediction is based on clinical evidence. Side effect risk increases with higher doses. Always consult your healthcare provider for personalized medical advice.
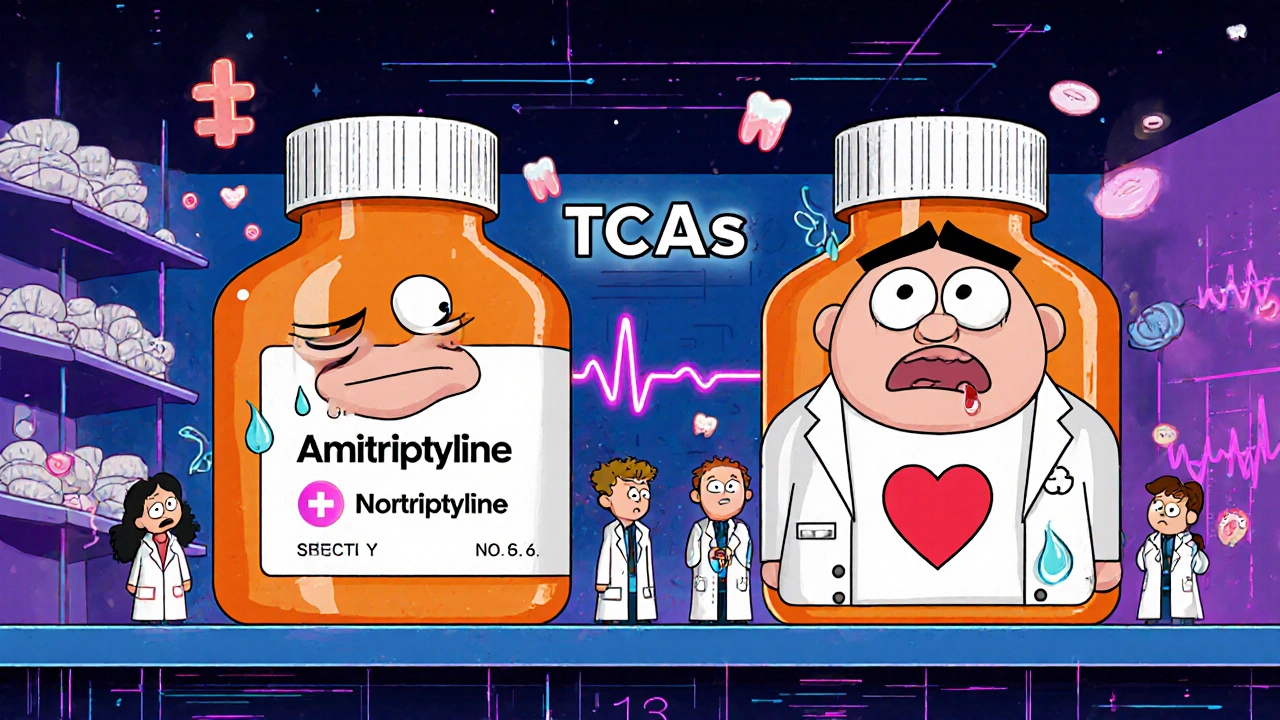
When you’re struggling with chronic pain, depression that won’t quit, or migraines that won’t leave you alone, doctors sometimes turn to older medications that still work-like amitriptyline or nortriptyline. These are part of a group called tricyclic antidepressants (TCAs), first developed in the 1950s. They’re not the go-to anymore, but for some people, they’re the only thing that brings real relief. The problem? Their side effects can be heavy, and not everyone can handle them.
How TCAs Work-and Why They Cause So Many Side Effects
Tricyclic antidepressants like amitriptyline and nortriptyline don’t just target one chemical in the brain. They block the reuptake of serotonin and norepinephrine, which helps lift mood. But they also stick to other receptors: cholinergic, histamine, and alpha-1 adrenergic. That’s why they cause dry mouth, drowsiness, blurry vision, and a racing heart. It’s not a bug-it’s how they’re built.
Amitriptyline, for example, binds tightly to muscarinic receptors (Ki = 1.8 nM), which control things like saliva production and bladder function. That’s why dry mouth affects up to 30% of users. Nortriptyline, its cousin, binds less tightly (Ki = 22.4 nM), so it’s often better tolerated. That’s why doctors sometimes switch patients from amitriptyline to nortriptyline when side effects become unbearable.
Common Side Effects You Can’t Ignore
Most people on TCAs will experience at least one of these common side effects within the first few weeks:
- Dry mouth - So common it’s almost expected. Up to 30% of people on amitriptyline report it. This isn’t just annoying-it leads to tooth decay, gum disease, and mouth infections if you don’t brush and floss daily.
- Blurred vision - Affects 15-20% of users. It usually clears up after a few weeks, but some people can’t drive safely during that time.
- Constipation - Happens in 20-25% of users. Slowed digestion can get dangerous if left unchecked. Laxatives help, but prevention (more water, fiber, movement) is better.
- Urinary retention - Especially risky for men with enlarged prostates. About 10-15% report trouble starting or maintaining urine flow. Some end up needing a catheter.
- Dizziness when standing - Called orthostatic hypotension. Your blood pressure drops suddenly when you stand up. That’s why people on TCAs often fall. Rising slowly helps, but it’s still a major risk for older adults.
- Fast heartbeat - Resting heart rate can jump 10-20 beats per minute. Not everyone notices it, but it’s a red flag for heart problems.
- Extreme drowsiness - Amitriptyline knocks out 40% of users. That’s why it’s usually taken at night. Nortriptyline is a bit gentler-around 25% feel sleepy.
These aren’t rare. They’re expected. And they’re why so many people quit TCAs within eight weeks. One study found 45% stopped because of side effects-compared to 25% for newer drugs like SSRIs.
The Real Dangers: Heart, Brain, and Overdose
Most side effects are annoying. But some can be life-threatening.
Heart risks are the biggest concern. TCAs can lengthen the QTc interval on an ECG-by 20 to 40 milliseconds with amitriptyline. That can trigger dangerous heart rhythms, even at normal doses. People with existing heart disease, high blood pressure, or a history of arrhythmias are at higher risk. The Lancet found TCAs carry a 35% higher risk of heart events than SSRIs.
Cognitive problems hit older adults hardest. About 25% of people over 65 on TCAs report confusion. Fifteen percent get disoriented. That’s why the Beers Criteria-used by doctors to avoid risky drugs in seniors-says to avoid amitriptyline completely in people over 65. Studies show a 70% higher risk of falls and a 50% higher risk of cognitive decline.
Overdose is terrifyingly easy. TCAs have a narrow safety margin. Taking just 2-3 times the daily dose can be fatal. Signs include a widened QRS complex on an ECG, low blood pressure, seizures, and breathing trouble. Death usually comes from heart failure or collapsed circulation. That’s why doctors keep prescriptions small and monitor patients closely.
Why Doctors Still Prescribe Them
If TCAs are so risky, why do they still exist?
Because for some conditions, they work better than anything else.
For neuropathic pain-like diabetic nerve pain or post-shingles pain-amitriptyline is the gold standard. A 2020 Cochrane Review showed it helped 35-40% of patients reduce pain by half. Duloxetine, a newer option, only helped 20-25%. That’s a big difference when you’re in constant pain.
For migraine prevention, amitriptyline cuts attack frequency by 70-80% in responders. One user on Healthgrades said: “After 10 years of 15 migraines a month, I’m down to 3.”
And for treatment-resistant depression-when SSRIs and SNRIs have failed-TCAs still deliver. A meta-analysis showed 65-70% of patients responded to TCAs after other meds didn’t work, compared to 50-55% with newer drugs.
So doctors don’t give them up. They just save them for when other options fail.
Amitriptyline vs. Nortriptyline: Which Is Better?
Not all TCAs are the same. Here’s how they stack up:
| Feature | Amitriptyline | Nortriptyline |
|---|---|---|
| Primary use | Depression, neuropathic pain, migraines | Depression, neuropathic pain (milder side effects) |
| Typical starting dose | 25-50 mg daily | 25 mg daily |
| Max daily dose | 150-200 mg | 100-150 mg |
| Sedation level | High (up to 40% of users) | Moderate (~25% of users) |
| Anticholinergic effects | Strong (dry mouth, constipation, blurred vision) | Milder |
| Cardiac risk | Higher | Lower |
| Best for | Pain, migraines, severe depression | Older adults, those sensitive to side effects |
Nortriptyline is often called the “cleaner” TCA. It’s metabolized from amitriptyline in the liver, and it doesn’t hit the same receptors as hard. That’s why it’s preferred for older patients or those with heart issues. But it’s not side-effect-free. You still get dry mouth, drowsiness, and dizziness-just less often.
Real People, Real Experiences
On Reddit, user “ChronicPainWarrior” wrote: “Amitriptyline finally helped my nerve pain after five other meds failed. But the dry mouth was so bad I went through three bottles of Biotene a day and still got two cavities. I switched to nortriptyline-better, but still tired all the time.”
On Drugs.com, amitriptyline has a 6.2/10 rating from over 1,800 reviews. The top complaints? “Cotton mouth,” “blurred vision made driving dangerous,” and “couldn’t pee without a catheter.”
But the positive stories are just as real. “After 10 years of migraines, amitriptyline cut my attacks from 15 to 3 per month,” said one user. “I gained 12 pounds, but I can finally leave the house.”
Weight gain is common-10-15 pounds in six months. Sexual side effects hit 35-40% of men. And “brain fog” shows up in nearly 30% of negative reviews.

How to Use TCAs Safely
If your doctor prescribes a TCA, here’s how to stay safe:
- Start low, go slow. Most doctors begin at 10-25 mg at bedtime. It takes 2-4 weeks to work. Don’t quit early because you feel worse at first.
- Take it at night. That helps with drowsiness and reduces fall risk.
- Rise slowly. Sit on the edge of the bed for 30 seconds before standing. Prevents dizziness.
- Brush and floss daily. Dry mouth is a dental disaster waiting to happen. Use sugar-free gum or Biotene.
- Get an ECG before starting. Especially if you have heart issues or are over 50.
- Don’t stop cold turkey. Withdrawal can cause electric shock sensations, nausea, and anxiety. Taper over 4-6 weeks.
- Watch for confusion or memory loss. Especially if you’re over 65. Tell your doctor immediately.
The American Psychiatric Association says TCAs should only be used after two failed trials of newer antidepressants. That’s not a suggestion-it’s a guideline based on safety.
Who Should Avoid TCAs?
TCAs are not for everyone. Avoid them if you:
- Have a history of heart attack, arrhythmia, or heart failure
- Are over 65 (especially with memory issues or risk of falls)
- Have glaucoma, enlarged prostate, or urinary retention
- Have liver disease (TCAs are processed in the liver)
- Are taking other drugs that affect heart rhythm (like certain antibiotics or antifungals)
- Have had a previous bad reaction to a TCA
And if you’re thinking about buying them online? Don’t. TCAs are dangerous without medical supervision. Even a small overdose can kill.
The Future of TCAs
TCAs are fading from first-line use. In 2022, they made up only 5-7% of all antidepressant prescriptions in the U.S.-down from 30% in the 1990s. But they’re not disappearing. Amitriptyline alone is still prescribed over 12 million times a year, mostly for pain.
New research is making them smarter. Combining low-dose amitriptyline (10-25 mg) with an SSRI can boost results while cutting side effects. Genetic testing is also helping: people with a CYP2D6 poor metabolizer gene break down amitriptyline slowly, leading to higher blood levels and worse side effects. Testing for this can prevent dangerous dosing.
Still, for some, TCAs are the last line of defense. As one psychiatrist put it: “When used carefully in the right person, they can change lives.”
But that’s the key: right person. Not everyone. Not always. Just when nothing else works-and you’re willing to manage the trade-offs.
Are tricyclic antidepressants still prescribed today?
Yes, but rarely as a first choice. Doctors now use them only after newer antidepressants like SSRIs or SNRIs have failed. They’re still commonly prescribed for neuropathic pain, migraines, and treatment-resistant depression-especially when other drugs don’t work. Amitriptyline remains one of the most prescribed generic drugs in the U.S., mostly for off-label pain use.
Which TCA has the fewest side effects?
Nortriptyline and desipramine tend to have fewer side effects than amitriptyline or imipramine. They’re called secondary amine TCAs and bind less strongly to receptors that cause dry mouth, drowsiness, and heart issues. That’s why they’re often preferred for older adults or people with heart conditions.
Can you drink alcohol while taking amitriptyline?
No. Alcohol increases drowsiness, dizziness, and the risk of falls. It also raises the chance of dangerous heart rhythm changes. Even small amounts can make side effects worse. Doctors strongly advise avoiding alcohol completely while on TCAs.
How long does it take for TCAs to work?
It usually takes 2 to 4 weeks before you feel the full effect. Some people notice small improvements in sleep or pain within the first week, but mood and pain relief take time. Stopping too soon because you don’t feel better right away is a common reason treatment fails.
Do TCAs cause weight gain?
Yes, weight gain is common. Most users gain 10-15 pounds in the first six months. This is due to increased appetite and slower metabolism caused by histamine blockade. Nortriptyline tends to cause less weight gain than amitriptyline, but it still happens.
Can TCAs be used safely in elderly patients?
Generally, no. The Beers Criteria recommends avoiding amitriptyline and other high-anticholinergic TCAs in people over 65. They increase the risk of confusion, falls, fractures, and cognitive decline. If absolutely necessary, nortriptyline at the lowest possible dose may be considered-but only with close monitoring.
What happens if you overdose on a TCA?
An overdose can be fatal. Symptoms include a widened QRS complex on ECG, severe low blood pressure, seizures, irregular heartbeat, and breathing failure. Death usually comes from cardiac arrest. Emergency treatment requires hospitalization, ECG monitoring, and sometimes sodium bicarbonate or activated charcoal. Never take more than prescribed.
Is it safe to stop taking TCAs suddenly?
No. Stopping abruptly can cause withdrawal symptoms like electric shock sensations, nausea, anxiety, insomnia, and rebound depression. Always taper off slowly over 4-6 weeks under medical supervision. Your doctor will help you reduce the dose gradually to avoid these effects.
TCAs are powerful tools-but they’re not for everyone. If you’re on one, know the risks. If you’re considering one, ask the questions. Your health depends on it.



Neoma Geoghegan
November 23, 2025 AT 17:33TCAs are a last-resort tool but when they click? Game changer for neuropathic pain. Just watch the QTc and hydrate like your life depends on it because it kinda does.
Bartholemy Tuite
November 23, 2025 AT 23:22Man i remember my uncle on amitriptyline back in the day. Dry mouth so bad he kept a water bottle taped to his wheelchair. Blurry vision made him miss his bus twice. But dude? His back pain vanished. He said it was like someone turned off a fire in his spine. Worth the side effects if you’re in that kind of hell. Still wouldn’t take it myself though. Too much like playing russian roulette with your heart.
Sam Jepsen
November 25, 2025 AT 05:08Just wanna say thank you for this breakdown. I’ve been on nortriptyline for 6 months for fibro pain and honestly didn’t realize how much of my brain fog was the med and not just chronic illness. Started taking it at 10mg, now at 25. Still sleepy but way less dry mouth than my buddy on amitriptyline. Also brushing twice a day with fluoride toothpaste and chewing xylitol gum. Saved my teeth. Small wins.
Yvonne Franklin
November 27, 2025 AT 03:04ECG before starting is non-negotiable. Saw a 72yo patient go into torsades after starting amitriptyline without one. They didn’t even know they had LQTS. Don’t be that person. Test first. Dose slow. Monitor.
Jessica Correa
November 28, 2025 AT 06:23I was skeptical but my neuro gave me nortriptyline after 3 failed SSRIs and honestly it cut my migraines in half. Yeah I’m tired and my mouth feels like the Sahara but I can finally go to work without hiding in a dark room. Worth it for me. Still avoid alcohol like it’s poison though.
manish chaturvedi
November 28, 2025 AT 22:24In India, TCAs are rarely prescribed due to availability and safety concerns. SSRIs dominate. But for those with chronic pain who have exhausted all options, amitriptyline remains a quiet hero. Still, we must emphasize caution, especially among elderly patients with comorbidities. Medical supervision is paramount.
Nikhil Chaurasia
November 29, 2025 AT 19:08I tried amitriptyline for 3 weeks. Couldn’t pee. Couldn’t sleep. Couldn’t see. And still felt like I was drowning in depression. I quit cold turkey because I thought I’d rather die than feel like a zombie with a dry mouth and a broken bladder. I know it works for some. Just not for me. And I’m not ashamed to say that.
Holly Schumacher
December 1, 2025 AT 07:51Everyone’s acting like TCAs are this mysterious magic bullet. No. They’re dangerous, archaic, and overprescribed for off-label use. The fact that 45% quit due to side effects means they’re not ‘working’ for most. And now we’re seeing a surge in cardiac events linked to off-label pain prescriptions. This isn’t treatment-it’s medical roulette. And the Beers Criteria exists for a reason. Stop normalizing this.
Michael Fitzpatrick
December 1, 2025 AT 16:49Just wanted to add something real. I’ve been on nortriptyline for 2 years now for chronic migraine and fibro. Yeah I gained 15 lbs and my memory’s not what it used to be. But I can hug my kids without crying from pain. I can walk the dog. I can sit through dinner without needing a nap. I don’t call it a miracle. I call it trade-offs. And I’m okay with that. If you’re considering it, talk to your doc about starting low. And if you get dry mouth? Get a humidifier. It’s not glamorous but it helps. You’re not alone in this.
Shawn Daughhetee
December 3, 2025 AT 11:01My grandma was on amitriptyline for neuropathy and she forgot her own birthday. Not joking. She thought she was 45 again. We pulled her off it and she was like a different person. So yeah it works for pain but the brain fog? That’s not just side effect. That’s brain damage waiting to happen. Please be careful.