Post-Surgery Eye Inflammation Symptom Checker
How to Use This Tool
Select all symptoms you observe in your child's eye after surgery. The tool will assess urgency based on medical guidelines and provide immediate next steps.
Select Symptoms Observed
Assessment Results
Select symptoms to see assessment
Next Steps
Why This Matters
Key Takeaways
- Redness, pain, and light sensitivity are the first clues that something’s wrong.
- Watch for discharge, swelling, fever, or any drop in vision within the first week after eye surgery.
- If any sign worsens or appears after 48 hours, call an eye doctor immediately.
- Simple home checks (like looking for pupil shape or tearing) can help you decide when to seek help.
- Early diagnosis prevents permanent damage and speeds up recovery.
What Is Postoperative Ocular Inflammation?
Postoperative ocular inflammation is a natural immune response that can occur after any eye operation, such as cataract extraction, strabismus correction, or retinal repair. The body releases chemicals to heal the surgical site, but sometimes the reaction becomes excessive, leading to redness, swelling, and pain.
In children, the signs can be subtle because they may not articulate discomfort the way adults do. Understanding the typical pattern of inflammation helps parents catch problems before they turn into infections or vision loss.
Why Children Are Different
Children have immune systems that react faster but also recover quicker than adults. Their eyes are smaller, making any swelling appear more dramatic. Moreover, children often rub their eyes, which can introduce bacteria and worsen inflammation.
Because of these factors, the window for safe observation is narrower-usually the first 72 hours after surgery.
Common Warning Signs to Watch For
Below are the most frequent clues that postoperative inflammation is happening:
- Red eye - a pink or blood‑shot appearance around the white of the eye.
- Pain - the child may squint, hold the eye shut, or complain of a dull ache.
- Photophobia - aversion to light; the child may cover their eyes or avoid bright rooms.
- Discharge - watery or mucous secretions that may crust around the lashes.
- Swelling of the eyelids or the area around the surgical site.
- Fever or general malaise, indicating the inflammation may be turning into an infection.
- Any sudden change in visual behavior (e.g., bumping into objects, trouble reading).
If you notice any of these, start a quick home assessment before calling the clinic.
Quick Home Assessment Checklist
- Observe the color of the sclera (the white part). Is it uniformly pink, or are there deep red patches?
- Ask the child to look at a bright light source. Do they wince or turn away?
- Gently pull back the lower eyelid to check for discharge or foreign material.
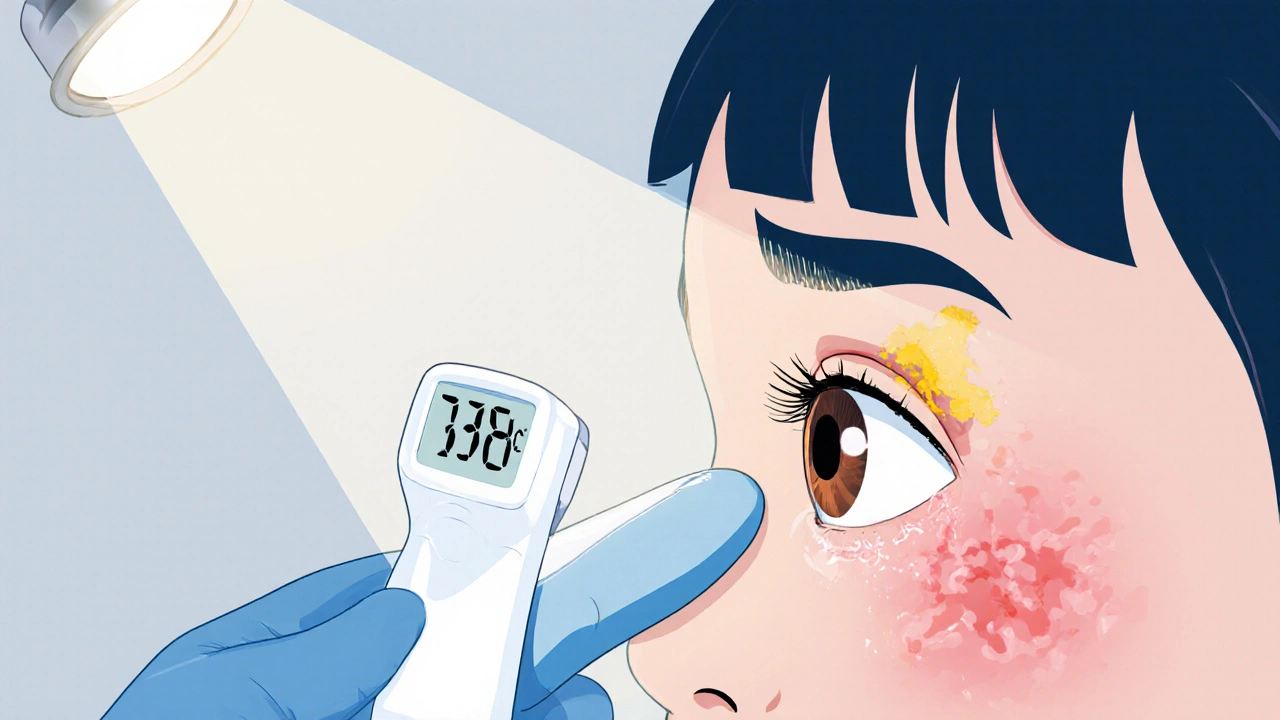
- Measure temperature. A fever above 38°C (100.4°F) combined with eye symptoms is a red flag.
- Check visual response: can the child track a moving object or identify simple pictures?
Document what you see-date, time, and any changes. This information speeds up the doctor’s evaluation.
When to Call an Eye Doctor
Ophthalmologist (eye doctor) should be contacted if any of the following occur:
- Redness spreads beyond the immediate surgical area.
- Pain escalates despite prescribed pain drops.
- Discharge becomes thick, yellow, or foul‑smelling.
- Fever develops or persists for more than 24 hours.
- Vision seems blurry, double, or the child can’t focus on objects.
Most clinics have an after‑hours line for postoperative concerns. Mention the surgery type and the exact symptoms when you call.
How Doctors Diagnose the Problem
During a follow‑up, the ophthalmologist may perform:
- Slit lamp examination - a magnified view that reveals cells, flare, or pus in the anterior chamber.
- Measurement of visual acuity using age‑appropriate charts.
- Intra‑ocular pressure testing to rule out secondary glaucoma.
- If infection is suspected, a tiny sample of discharge may be cultured.
Based on findings, the doctor may prescribe topical steroids to calm inflammation, antibiotics for bacterial involvement, or adjust existing eye drops.
Home Care Tips While Waiting for the Appointment
- Apply a cold compress (clean cloth soaked in cool water) for 5‑10 minutes, three times a day, to reduce swelling.
- Maintain strict hand hygiene; wash hands before touching the eye or applying drops.
- Administer prescribed eye drops exactly as directed-never skip a dose.
- Keep the child’s head elevated during sleep to lessen fluid buildup.
- Avoid irritants like smoke, dust, or bright screens until the eye settles.
These measures help control the inflammation and prevent secondary infection.

Potential Complications If Left Unchecked
Uncontrolled postoperative inflammation can lead to:
- Corneal scarring, which permanently blurs vision.
- Secondary glaucoma-a rise in eye pressure that threatens optic nerve health.
- Endophthalmitis, a serious internal eye infection that requires intravenous antibiotics.
Prompt treatment dramatically lowers the risk of these outcomes. That’s why the phrase postoperative eye inflammation should trigger immediate action.
Comparison of Common Signs and Their Typical Timing
| Sign | Usually appears | Urgency level |
|---|---|---|
| Mild redness | Within 12‑24 hrs | Low - monitor |
| Moderate pain | 24‑48 hrs | Medium - call doctor if worsens |
| Thick yellow discharge | 24‑72 hrs | High - seek urgent care |
| Fever >38°C | Any time | High - immediate evaluation |
| Blurred vision | 48‑72 hrs | High - urgent assessment |
Bottom‑line Checklist for Parents
- Record the time of surgery and any prescribed drops.
- Check the eye twice daily for redness, swelling, or discharge.
- Take the child’s temperature each evening for the first three days.
- Note any changes in behavior: irritability, rubbing, or difficulty seeing.
- Call the ophthalmology clinic immediately if any high‑urgency sign appears.
Frequently Asked Questions
How long does normal postoperative redness last?
Mild pinkness can persist for up to three days. It should gradually fade and never become deep red or spread to the entire eye.
Are eye drops enough to control inflammation?
Often yes, especially steroid or non‑steroidal drops prescribed after surgery. However, if swelling or pain continues, a doctor may add oral medication or a stronger topical preparation.
Can a child’s eye heal on its own without medication?
Mild inflammation may subside with rest and a cold compress, but most surgeons recommend a short course of prescribed drops to avoid scarring.
What should I do if the child accidentally rubs the eye?
Clean the hands immediately, apply a sterile saline rinse if any foreign material appears, and monitor for increased redness or discharge. Contact the clinic if irritation spikes.
Is fever a sign of infection or just inflammation?
Fever usually points to infection, especially when paired with thick discharge. Even low‑grade fever warrants a prompt call to the ophthalmologist.





Megan Lallier-Barron
October 12, 2025 AT 05:04Life’s little inflammations teach us that the body’s fire is both guardian and rebel 🌱.
When a child’s eye turns crimson after surgery, it whispers a warning we can’t ignore.
Yet, we often chase the calm before the storm, forgetting that discomfort is a signal, not a failure.
Observing the pupil’s shade, the child’s aversion to light, and any sudden fever is the quiet poetry of healing.
If the poem turns dark, a doctor’s call becomes the stanza we need. 😊
Kelly Larivee
October 20, 2025 AT 06:36The checklist is easy to follow and saves a lot of worry.
Just keep an eye on redness and fever for the first few days.
Emma Rauschkolb
October 28, 2025 AT 07:09Post‑operative ocular inflammation engages a cascade of cytokines, chemokines, and vascular permeability – the immunologic orchestra that can crescendo into endophthalmitis 😬.
Discharge that shifts from serous to purulent indicates a microbial takeover, demanding immediate antimicrobial intervention.
Photophobia signifies corneal edema disrupting the refractive front, thereby impairing visual acuity.
A febrile response >38 °C synergizes with intra‑ocular pressure spikes, flagging secondary glaucoma.
Monitoring these biomarkers transforms parental vigilance into a quasi‑clinical protocol. 😉
Kaushik Kumar
November 5, 2025 AT 08:41Great job on tracking the symptoms so far!
Keep the cold compress on for 5‑10 minutes, three times a day!!!
Remember, hand hygiene is the cornerstone of infection control!!!
If pain worsens despite drops, ring the clinic without delay!
Mara Mara
November 13, 2025 AT 10:14Our pediatric eye care standards are among the best worldwide; trust the protocol.
Immediate reporting of high‑urgency signs aligns with top‑tier ophthalmology guidelines.
Your vigilance protects the child’s vision and our national health reputation.
Jennifer Ferrara
November 21, 2025 AT 11:46It is of utmost importence to recognise that the subtile hue of sclera may belie a deeper pathology.
While mild redness can be part of the normal healing cascade, a sudden intensification warrants immediate consult.
The presence of fever, however modest, may suggest an infectious etiology requiring prompt antimicrobial therapy.
Thus, a measured yet swift response is advised.
Terry Moreland
November 29, 2025 AT 13:19I understand how stressful this can be for both you and your little one.
Keep the eyelid clean, apply the prescribed drops exactly as ordered, and watch for any change in behavior.
If anything feels off, don’t hesitate to call your doctor.
Abdul Adeeb
December 7, 2025 AT 14:51Your emphasis on precise observation is commendable; however, it is crucial to note that the term “subtle hue” may be misinterpreted by laypersons.
Clarifying that a mild pinkish tint is normal, whereas a deep crimson suggests pathology, would enhance comprehension.
Additionally, specifying the timeframe for expected resolution would be beneficial.
Abhishek Vernekar
December 15, 2025 AT 16:24Indeed, clear guidance eliminates ambiguity, and a concise timeline aids parental decision‑making.
A simple table distinguishing normal from concerning signs could serve as an effective visual aid.
Let’s ensure the language remains both accurate and accessible.
Val Vaden
December 23, 2025 AT 17:57Just remember, the eyes don’t lie - call the doc if they start to stink. 😒
lalitha vadlamani
December 31, 2025 AT 19:29To neglect a child’s inflamed eye is to gamble with destiny, a transgression that stains the very soul of caregiving.
One must rise above complacency, wielding knowledge as a shield against needless suffering.
The moral imperative is clear: vigilance today prevents irreversible blindness tomorrow.
Let us not be the architects of regret.
kirk lapan
January 8, 2026 AT 21:02While the checklist presented is thorough, it omits the nuance of differential diagnosis between sterile inflammation and infectious endophthalmitis, a distinction that hinges on the character of discharge and intra‑ocular pressure measurements.
Moreover, the recommendation to “call within the next hour” fails to account for regional clinic availability, potentially causing unnecessary panic.
A tiered response algorithm, incorporating telemedicine triage, would mitigate these shortcomings.
In practice, the timing of intervention can be the difference between full recovery and permanent visual deficit.
Thus, a more granular protocol is advisable.
Vince D
January 16, 2026 AT 22:34Your summary hits the key points succinctly; great job.
Collaboration on patient education will only improve outcomes.
Ian Frith
January 25, 2026 AT 00:07When a child's eye becomes inflamed after surgery, the clock starts ticking louder than any alarm.
Each hour without proper intervention raises the stakes, turning a manageable irritation into a perilous battlefield.
First, observe the color of the sclera; a uniform pink is a sign of healing, whereas deep ruby indicates vascular leakage.
Next, test light tolerance: a child who flinches at a bedside lamp is signaling photophobia, a red flag for corneal involvement.
Check for discharge; a thin watery stream may be normal, but thick yellow or foul‑smelling material is the hallmark of bacterial invasion.
Measure temperature; fever above 38 °C coupled with ocular symptoms suggests systemic infection that must be addressed immediately.
Assess vision by tracking a favorite toy; any hesitancy or loss of focus points to possible intra‑ocular pressure spikes.
Document every observation with timestamps; this log becomes the narrative that guides the ophthalmologist's diagnosis.
Apply a sterile cold compress for five minutes, three times daily, to quell swelling without compromising circulation.
Maintain hand hygiene rigorously; germs travel faster than you think, especially when a child rubs the eye.
Administer prescribed steroid drops exactly as scheduled; skipping doses can provoke rebound inflammation.
If pain intensifies despite medication, it is an unequivocal signal to seek urgent care, even if other signs seem mild.
Remember, the window for preventing permanent corneal scarring is narrow-typically within the first 72 hours post‑op.
Should an infection be confirmed, systemic antibiotics may be required alongside topical therapy to halt progression.
In summary, vigilant monitoring, swift action, and strict adherence to the care plan are the triumvirate that safeguards a child's vision.
Beauty & Nail Care dublin2
February 2, 2026 AT 01:39Ever notice how these “official” tools claim to be neutral while silently pushing a hidden agenda?
They collect data on every symptom you select, feeding algorithms that favor big‑pharma solutions.
It’s almost as if the tool wants you to call the clinic sooner, ensuring more appointments and prescriptions.
Stay skeptical, question the motives behind the urgency badges, and trust your own observations first.
Remember, the most powerful diagnostics are the ones you perform yourself, not the ones baked into a website.
Oliver Harvey
February 10, 2026 AT 03:12Oh, because the internet magically knows when a child’s eye is about to explode, right?
Sure, let’s all ignore professional advice and rely on a checkbox wizard.
If you enjoy living on the edge, keep ignoring the doctor’s orders.
Ben Poulson
February 18, 2026 AT 04:04The outlined protocol adheres to established ophthalmic guidelines and presents the information with commendable clarity.
Implementation of the recommended monitoring schedule should enhance early detection of postoperative complications.