Medication Selection Assistant
Find Your Best Medication Option
Answer a few questions to get a personalized recommendation based on current medical guidelines.
When a doctor prescribes a calcium‑channel blocker, many patients wonder how Diltiazem stacks up against the other options on the market. This guide walks through the most common alternatives, highlights where each shines, and points out the trade‑offs you’re likely to meet in real‑world use.
Key Takeaways
- Diltiazem blends heart‑rate control with vasodilation, making it a go‑to for angina and certain types of hypertension.
- Amlodipine offers smoother blood‑pressure control but can cause ankle swelling.
- Verapamil is the strongest heart‑rate depressant but interacts heavily with other heart meds.
- Nifedipine works fast for acute pressure spikes but may trigger reflex tachycardia.
- Choosing the right drug depends on the primary condition, side‑effect tolerance, and other medicines you take.
What is Diltiazem HCl?
Diltiazem HCl is a benzothiazepine calcium‑channel blocker that relaxes smooth muscle in blood vessels and the heart. It was first approved in the early 1990s and quickly became a staple for treating chronic stable angina, atrial fibrillation rate control, and hypertension that needs both vasodilation and heart‑rate reduction. Typical oral doses range from 30mg to 480mg per day, split into once‑ or twice‑daily dosing. Its dual action makes it unique among calcium‑channel blockers, which usually fall into either the dihydropyridine (vascular‑selective) or non‑dihydropyridine (cardiac‑selective) families.
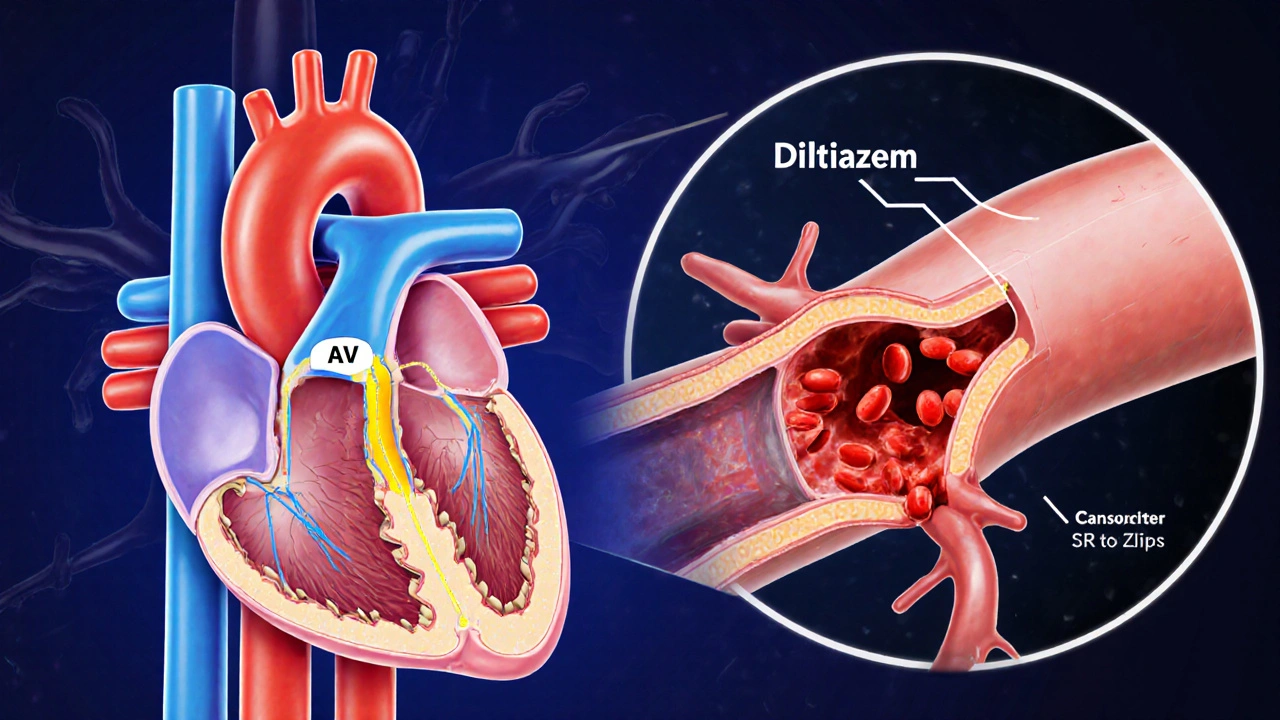
How Diltiazem Works (Mechanism of Action)
Diltiazem blocks L‑type calcium channels in both vascular smooth muscle and the cardiac conduction system. By limiting calcium influx, it reduces contractile force in arteries (lowering systemic vascular resistance) and slows electrical conduction through the AV node (controlling heart rate). This combined effect explains why it is often chosen when a patient needs both blood‑pressure reduction and rhythm control.
Major Alternatives to Diltiazem
Below are the most widely used drugs that sit in the same therapeutic space. Each entry starts with a brief definition marked up with microdata for easy knowledge‑graph extraction.
Amlodipine is a dihydropyridine calcium‑channel blocker primarily targeting peripheral arteries. It provides steady blood‑pressure control, especially in patients with isolated systolic hypertension. Common doses range from 2.5mg to 10mg once daily.
Verapamil is a non‑dihydropyridine calcium‑channel blocker that leans heavily toward cardiac effects, making it a strong AV‑node depressor. It is prescribed for angina, supraventricular tachycardia, and certain cases of hypertension. Typical oral dosing is 80mg to 480mg per day, divided into 2‑3 doses.
Nifedipine is a rapid‑acting dihydropyridine used for acute blood‑pressure spikes and severe angina. Immediate‑release formulations start at 10mg three times daily, while extended‑release versions range from 30mg to 60mg once daily.
Atenolol is a beta‑blocker that reduces heart rate and contractility without directly affecting vascular tone. It’s a standard choice for hypertension and post‑myocardial‑infarction care. Usual doses are 25mg to 100mg once daily.
Lisinopril is an ACE inhibitor that lowers blood pressure by preventing angiotensin‑II formation, leading to vasodilation and reduced aldosterone‑mediated volume retention. Doses typically start at 5mg and can go up to 40mg daily.
Direct Comparison Table
| Drug | Class | Primary Indication | Typical Dose | Common Side Effects | Notable Interactions |
|---|---|---|---|---|---|
| Diltiazem HCl | Non‑dihydropyridine calcium‑channel blocker | Angina, atrial fibrillation rate control, hypertension | 30‑480mg/day (split) | Bradycardia, edema, constipation | CYP3A4 inhibitors (e.g., ketoconazole) |
| Amlodipine | Dihydropyridine calcium‑channel blocker | Hypertension, stable angina | 2.5‑10mg/day | Ankle swelling, flushing, headache | Cyclosporine (increases levels) |
| Verapamil | Non‑dihydropyridine calcium‑channel blocker | Angina, supraventricular tachycardia, hypertension | 80‑480mg/day (split) | Constipation, bradycardia, AV block | Beta‑blockers (risk of severe bradycardia) |
| Nifedipine (ER) | Dihydropyridine calcium‑channel blocker | Hypertension, angina | 30‑60mg/day | Headache, peripheral edema, reflex tachycardia | Grapefruit juice (CYP3A4 inhibition) |
| Atenolol | Beta‑blocker | Hypertension, post‑MI, arrhythmias | 25‑100mg/day | Fatigue, cold extremities, bronchospasm | Calcium‑channel blockers (additive heart‑rate lowering) |
| Lisinopril | ACE inhibitor | Hypertension, heart failure | 5‑40mg/day | Cough, hyperkalemia, angioedema | Potassium‑sparing diuretics (hyperkalemia risk) |
When Diltiazem Is the Better Choice
If your primary problem is a combination of high blood pressure and a fast heart rate (as in atrial fibrillation), Diltiazem’s dual action can simplify therapy. It also has a more predictable effect on AV‑node conduction than Amlodipine, which barely influences heart rate. For patients with peripheral arterial disease who need vasodilation without causing a sudden drop in blood pressure, Diltiazem’s moderate vasodilatory profile is a safer middle ground.
When One of the Alternatives Might Win
Amlodipine shines when you need steady, once‑daily blood‑pressure control and you’re less concerned about heart‑rate changes. Its long half‑life reduces pill burden, which improves adherence for older adults. However, the trade‑off is a higher chance of ankle swelling, especially in patients already on diuretics.
Verapamil is preferred for controlling ventricular response in atrial flutter or for patients who cannot tolerate beta‑blockers. Its potent AV‑node suppression can be a lifesaver in certain arrhythmias, but the same potency raises the risk of severe bradycardia if combined with other rate‑slowing agents.
Nifedipine (especially the extended‑release form) works fast for hypertensive emergencies and is a solid choice for patients who need rapid symptom relief from angina. The downside is reflex tachycardia, which can be problematic for people with existing tachyarrhythmias.
Beta‑blockers like Atenolol remain first‑line for post‑myocardial‑infarction patients because they cut mortality risk-not something calcium‑channel blockers can claim. If a patient also has asthma, a cardioselective beta‑blocker may still be viable, whereas non‑selective options provoke bronchospasm.
ACE inhibitors such as Lisinopril are the go‑to for chronic kidney disease patients because they protect renal function. Their cough side effect can be limiting, driving some clinicians toward ARBs or calcium‑channel blockers when tolerance becomes an issue.
Side‑Effect Profiles at a Glance
Side effects often dictate which drug a clinician finally picks. Below is a concise rundown:
- Diltiazem: Bradycardia, constipation, peripheral edema (less common than in dihydropyridines).
- Amlodipine: Ankle swelling, flushing, dizziness.
- Verapamil: Constipation, severe bradycardia, AV block.
- Nifedipine: Headache, reflex tachycardia, flushing.
- Atenolol: Fatigue, cold extremities, may mask hypoglycemia.
- Lisinopril: Persistent cough, angioedema, hyperkalemia.
Drug Interactions You Can’t Ignore
Because many of these agents are metabolized by the liver’s CYP3A4 system, concomitant use of strong inhibitors (like ketoconazole or certain macrolide antibiotics) can raise plasma concentrations dramatically. For example, adding a CYP3A4 inhibitor to Diltiazem often necessitates a dose cut‑back of 50% to avoid heart‑block risks.
Combining two rate‑slowing drugs-such as Diltiazem with a beta‑blocker or Verapamil-requires careful ECG monitoring. The same caution applies when pairing ACE inhibitors with potassium‑sparing diuretics, which can push serum potassium into dangerous territory.
Practical Decision‑Making Checklist
- Is the main goal blood‑pressure control alone? → Consider Amlodipine or Lisinopril.
- Do you need heart‑rate reduction (e.g., atrial fibrillation)? → Diltiazem or Verapamil are top picks.
- Is rapid symptom relief essential (e.g., acute angina)? → Nifedipine ER or short‑acting Diltiazem.
- Does the patient have a history of asthma, COPD, or renal impairment? → Lean toward Diltiazem or Amlodipine, avoid beta‑blockers or ACE inhibitors respectively.
- Are there known CYP3A4 inhibitors in the regimen? → Adjust Diltiazem or Verapamil dose, or choose a non‑CYP3A4‑metabolized option.
Real‑World Example Scenarios
Scenario 1 - A 62‑year‑old with hypertension and newly diagnosed atrial fibrillation
The cardiologist opts for Diltiazem 120mg twice daily because it lowers blood pressure while keeping the ventricular rate around 70bpm. After six weeks, the patient reports mild ankle swelling, which is managed by adding a low‑dose thiazide diuretic rather than switching drugs.
Scenario 2 - A 55‑year‑old with isolated systolic hypertension and chronic kidney disease stage3
Lisinopril 20mg daily is chosen for its renal‑protective effect. The patient later develops a dry cough; the physician switches to Diltiazem 60mg twice daily, which successfully controls systolic pressure without compromising kidney function.
Scenario 3 - A 48‑year‑old marathon runner experiencing exertional angina
Because the runner’s heart rate is already high, Verapamil is avoided. Instead, a low‑dose Amlodipine 5mg daily is started to improve coronary perfusion without further slowing the heart. The runner notices reduced chest discomfort within two weeks.
Bottom Line: Tailor the Choice to the Patient
There’s no one‑size‑fits‑all answer. Diltiazem’s hybrid profile makes it a strong contender when both blood‑pressure and heart‑rate need attention. If you only need vascular dilation, Amlodipine or an ACE inhibitor may be simpler. When rhythm control dominates, Verapamil or a beta‑blocker could be superior. Always weigh the side‑effect landscape, drug‑interaction potential, and the patient’s comorbidities before settling on a regimen.
Frequently Asked Questions
What conditions is Diltiazem primarily prescribed for?
Diltiazem is most often used to treat chronic stable angina, control ventricular rate in atrial fibrillation or flutter, and manage hypertension that benefits from both vasodilation and heart‑rate reduction.
How does Diltiazem differ from Amlodipine?
Amlodipine belongs to the dihydropyridine class and mainly relaxes arterial smooth muscle, leaving heart rate largely unchanged. Diltiazem, as a non‑dihydropyridine, also slows AV‑node conduction, making it useful for rhythm control.
Can Diltiazem be taken with a beta‑blocker?
Yes, but the combination can cause pronounced bradycardia or AV‑block. Physicians usually start both at low doses and monitor heart rate and ECG closely.
What are the most common side effects of Diltiazem?
Patients often notice mild constipation, occasional peripheral edema, and in some cases, a slower-than‑desired heart rate. Most side effects are dose‑dependent and improve with adjustment.
Is Diltiazem safe during pregnancy?
Animal studies have not shown major teratogenic effects, but human data are limited. The medication should only be used if the potential benefit outweighs the risk, and usually under specialist guidance.






Lawrence Bergfeld
October 13, 2025 AT 12:39Keep your dosage consistent, monitor your pulse regularly, and report any swelling to your provider immediately!
Othilie Kaestner
October 17, 2025 AT 05:16Honestly, the hype around diltiazem is overrated; most patients do just fine on cheaper blood pressure pills.
Sebastian Samuel
October 20, 2025 AT 21:53😅 But skipping the heart‑rate control? That's a gamble you shouldn't take, especially if you love marathon runs! 🚀
Brandon Smith
October 24, 2025 AT 14:30From an ethical standpoint, prescribing a medication with a dual mechanism like diltiazem demands careful justification; the clinician must weigh the benefit of rate control against the risk of bradycardia. Moreover, the literature consistently shows that inappropriate combination with beta‑blockers can precipitate serious conduction disturbances.
april wang
October 28, 2025 AT 06:07When we look at the pharmacologic profile of diltiazem, the first point to acknowledge is its classification as a non‑dihydropyridine calcium‑channel blocker, which inherently gives it both vasodilatory and negative dromotropic properties; this dual action makes it uniquely suited for patients who present with both hypertension and a tachyarrhythmic component.
In clinical practice, the decision to start diltiazem often follows a thorough assessment of comorbid conditions such as chronic kidney disease, where its relatively renal‑sparing metabolism can be advantageous compared with ACE inhibitors.
Conversely, patients with a history of severe heart failure may require closer monitoring because the negative inotropic effect, while modest, can exacerbate symptoms if dosing is not titrated carefully.
Another dimension to consider is drug‑drug interaction potential; the agent is metabolized primarily by CYP3A4, so concomitant use of strong inhibitors like ketoconazole mandates a dose reduction to avoid excessive serum concentrations that could precipitate bradyarrhythmias.
From a side‑effect perspective, the most common complaints are peripheral edema and constipation, both of which are generally dose‑dependent and often manageable with adjunctive therapies such as low‑dose diuretics or stool softeners.
Patients frequently compare diltiazem to its dihydropyridine counterparts, notably amlodipine, noting that while amlodipine provides smoother blood‑pressure control, it lacks the rate‑controlling benefits that are clinically valuable in atrial fibrillation.
In the setting of angina, diltiazem’s capacity to reduce myocardial oxygen demand by lowering heart rate can translate into fewer anginal episodes, a therapeutic advantage that is not shared by pure vasodilators.
It is also worth mentioning that extended‑release formulations of diltiazem improve adherence by allowing once‑daily dosing, yet they require careful timing with meals to ensure consistent absorption.
Cost considerations are not negligible; while generic diltiazem is relatively inexpensive, the price differential with newer agents can influence formulary decisions in certain healthcare systems.
From a patient‑education standpoint, emphasizing the importance of regular blood‑pressure and heart‑rate monitoring can empower individuals to recognize early signs of over‑suppression, such as dizziness or syncope.
Clinicians should also counsel patients on the risks of grapefruit juice, which can inhibit CYP3A4 and inadvertently raise diltiazem levels, potentially leading to adverse cardiac effects.
In summary, the selection of diltiazem should be individualized, balancing its dual therapeutic benefits against its side‑effect profile and interaction landscape, with regular follow‑up to fine‑tune the regimen.
Ultimately, when used judiciously, diltiazem remains a cornerstone in the management of combined hypertensive and arrhythmic disorders, offering a practical compromise between efficacy and tolerability.
Vishnu Raghunath
October 31, 2025 AT 22:44Sure, because the government probably invented diltiazem to control our hearts like little drones.
Aparna Dheep
November 4, 2025 AT 15:21Diltiazem's place in therapy is unquestionable, yet many fail to grasp its nuanced pharmacodynamics which, frankly, elevate it above most generic options
Nicole Powell
November 8, 2025 AT 07:58The only thing more pretentious than a discussion about diltiazem is the way some people treat their own opinions as gospel.
Ananthu Selvan
November 12, 2025 AT 00:35Honestly this whole diltiazem debate is just noise ignore it
Nicole Chabot
November 15, 2025 AT 17:11I'm curious about how the dosing schedule changes when a patient switches from immediate‑release to extended‑release diltiazem.
Sandra Maurais
November 19, 2025 AT 09:48While the data undeniably support the efficacy of diltiazem, it is essential to approach its application with rigorous scrutiny, especially regarding polypharmacy; 📊
Rajan Desai
November 23, 2025 AT 02:25Could anyone clarify the impact of renal impairment on diltiazem clearance and whether dose adjustments are truly necessary?
S O'Donnell
November 26, 2025 AT 19:02In considiration of the extant pharmocological literature, it is paramount to distingush betwen the pharmacokinetic profiles of immediate‑release versus extended‑release diltiazem; the former necessitates ae more frequent dosing which may inadvertently compromise patient adherance, wheras the latter, despite its convenience, imposes a higher half‑life which could potentiate accumulation in cases of hepatic insufficieny – ths nuance is oft overlooked in clinical practice.
Yamunanagar Hulchul
November 30, 2025 AT 11:39What a dazzling array of options! 🌟 Diltiazem shines like a sunrise over the therapeutic horizon, offering both heart‑rate control and blood‑pressure relief-truly a champion for those seeking balance!