Naloxone Co-Prescribing Calculator
Morphine Milligram Equivalent Calculator
Calculate morphine milligram equivalents for opioid medications to determine if naloxone co-prescribing is recommended.
Current MME Calculation
0 MME/day
Click "Add Medication" to calculate MME
Naloxone Co-Prescribing Guidance
Important Notes
This calculator helps you assess risk but doesn't replace clinical judgment. Always consider all risk factors including concurrent benzodiazepines, substance use disorder history, and respiratory conditions.
When an opioid prescription crosses the line from pain relief to danger, having a safety net can mean the difference between life and death. Naloxone co-prescribing puts that net right in the patient’s pocket - a simple, evidence‑based step that lets families and caregivers reverse an overdose before emergency services arrive.
Quick Takeaways
- Co‑prescribe naloxone for any patient on ≥50 MME/day, with benzodiazepines, or with a history of substance use disorder.
- Use the CDC’s MME calculator to verify dosage thresholds.
- Choose the formulation that fits the patient’s setting - intranasal spray is the easiest for non‑clinical caregivers.
- Document risk assessment, education, and dispensing in the EHR to meet state and payer requirements.
- Expect a 40‑60% reduction in opioid‑related emergency visits when implementation is consistent.
What Exactly Is Naloxone Co‑Prescribing?
Naloxone co‑prescribing is the practice of issuing a naloxone kit at the same time an opioid analgesic is prescribed to a patient who meets defined risk criteria. The goal is to ensure that a rescue medication is available to the patient, a family member, or any bystander the moment an overdose begins. It emerged from the 2016 CDC Guideline (Recommendation 8) after the United States saw nearly 48,000 opioid‑related deaths in 2017.
Why It Matters: The Evidence Behind the Practice
Several large studies confirm the impact:
- A 2019 Annals of Internal Medicine analysis of 1,985 primary‑care patients showed a 47% drop in emergency‑department visits and a 63% cut in hospitalizations when naloxone was co‑prescribed.
- National data from the CDC’s 2023 Vital Signs report noted a 114% increase in naloxone dispensing between 2017‑2018, coinciding with a modest dip in overdose mortality.
- Dr. Wilson Compton (NIH) testified that every 10% rise in naloxone distribution correlates with a 1.2% reduction in opioid‑related deaths.
These numbers aren’t just statistics; they translate into real families saved from tragedy.
Key Risk Factors that Trigger Co‑Prescribing
The CDC and HHS outline a short list of clinical flags. If any appear, the clinician should discuss naloxone and offer a prescription.
- Opioid dosage ≥50 morphine‑milligram equivalents (MME) per day.
- Concurrent benzodiazepine prescription, regardless of opioid dose.
- History of non‑fatal overdose within the past year.
- Diagnosed substance‑use disorder (opioid or non‑opioid).
- Respiratory comorbidities such as COPD or obstructive sleep apnea.
- Significant alcohol use or chronic mental‑health conditions.
- Recent release from incarceration or residential treatment, where tolerance may be reduced.
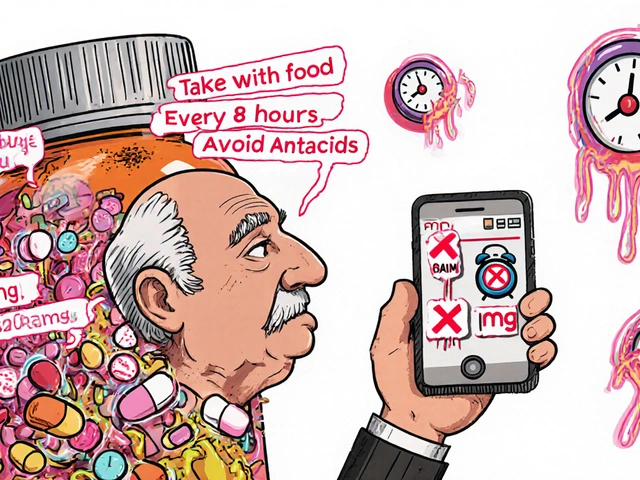
How to Calculate MME - The CDC Calculator
MME conversion is the linchpin of any risk assessment. The CDC provides an online calculator, but the core formula is simple:
- Oral morphine dose × 1 = MME.
- Oral oxycodone × 1.5 = MME.
- Oral hydrocodone × 1 = MME.
- Transdermal fentanyl (mcg/hr) × 2.4 = MME.
For example, 30 mg of oral morphine equals 30 MME, while 30 mg of oxycodone equals 45 MME.

Choosing the Right Naloxone Formulation
Four FDA‑approved formats exist, each with pros and cons:
| Formulation | Route | Typical Dose | Ease of Use | Cost (2023) |
|---|---|---|---|---|
| Narcan® nasal spray | Intranasal | 2 mg (single spray) | Very easy - press‑and‑hold | $130‑$150 (brand) |
| Generic nasal spray | d>Intranasal | 2 mg | Easy - similar device | $25‑$50 |
| Injectable kit (1 mg vials) | Intramuscular / Sub‑Q | 0.4 mg IM (0.4 mL) | Requires needle; more training | $20‑$35 |
| Kloxxado™ high‑dose nasal | Intranasal | 8 mg | Easy, higher potency for fentanyl‑heavy overdoses | $180‑$210 |
For most patients and caregivers, the intranasal spray (generic if insurance permits) offers the best balance of speed, simplicity, and acceptance.
Step‑by‑Step Workflow for Clinicians
The CDC’s implementation guide breaks the process into three quick steps that take about five minutes per at‑risk patient.
- Risk Assessment: Pull the state PDMP, check for high MME, benzodiazepines, or recent overdose. Document the findings in a dedicated EHR field.
- Patient Education: Use the SAMHSA “S.L.A.M.” framework - Signs, Life‑saving steps, Administer, Monitor. Hand the patient a one‑page flyer and walk through a real‑life scenario.
- Prescription & Dispensing: Write the naloxone prescription, attach dosage instructions, and arrange for pharmacy pickup or direct dispensing from the clinic’s stock. Verify insurance coverage or apply the standing order if the patient is uninsured.
Documenting each step satisfies most state mandates and eases prior‑authorisation delays.
Overcoming Common Barriers
Even with clear guidelines, clinicians hit snags:
- Patient stigma: Many refuse naloxone because they feel “labeled” as addicts. Using motivational interviewing - ask, reflect, summarize - softens the conversation.
- Provider discomfort: 68% of physicians admit they find overdose discussions awkward. Role‑play with a colleague or use the CDC’s scripted talking points to build confidence.
- Insurance hurdles: Prior to the SUPPORT Act, many plans required copays. Today, most insurers cover naloxone with little or no cost, but verify the formulary and use the generic version whenever possible.
- Pharmacy stock: Rural pharmacies only stocked naloxone 42% of the time in 2023. Consider clinic‑based dispensing or a standing order that lets the patient pick up at any pharmacy.
State‑Level Mandates - A Quick Snapshot
Regulations differ across the U.S. As of September 2024, 24 states have explicit co‑prescribing requirements. The table below highlights the most common thresholds.
| State | Threshold | Mandatory Offer? | Notes |
|---|---|---|---|
| California (AB 1386) | ≥90 MME/day | Yes | Includes patients on benzodiazepines. |
| New York | Any opioid prescription | Yes | Broadest mandate in the nation. |
| Illinois | ≥50 MME/day or concurrent benzo | Yes | Requires documentation of counseling. |
| Texas | ≥70 MME/day | Only if patient has prior overdose. | |
| Florida | ≥50 MME/day | Yes | Pharmacist can dispense under standing order. |
Clinicians practicing across state lines should adopt the most stringent rule (often New York’s “any dose” standard) to stay safe.

Real‑World Stories: What Happens When It Works
Sarah Johnson, a chronic‑pain patient in Ohio, recalls the day her teenage son mistook her oxycodone tablets for vitamins. “I was terrified, but the nasal spray saved his life within minutes,” she says. In Kentucky, Dr. Michael Chen reported 17 documented overdose reversals by family members after his clinic made co‑prescribing routine for anyone on >50 MME/day.
These anecdotes echo the data: when naloxone lands in the hands of a trusted caregiver, the window for emergency‑room intervention shrinks dramatically.
Future Directions - What’s Coming Next?
Funding and research pipelines suggest three trends:
- Long‑acting naloxone: A Phase III trial (NCT04875435) aims to deliver a month‑long protective level, potentially reducing the need for repeat kits.
- Community‑based distribution: The 2023 HHS grant program will place 1.2 million kits in harm‑reduction sites, expanding reach beyond clinic patients.
- Digital risk tools: Integrated EHR alerts that auto‑calculate MME and suggest a naloxone order are rolling out in major health‑system networks.
Staying abreast of these changes ensures clinicians can keep the safety net strong.
Quick Checklist for Providers
- Verify opioid dose with the CDC MME calculator.
- Screen for the seven CDC risk factors.
- Discuss naloxone using the S.L.A.M. script.
- Prescribe the most accessible formulation (generic nasal spray if covered).
- Document risk, education, and dispensing in the EHR.
- Follow state‑specific mandates - err on the side of broader coverage.
Frequently Asked Questions
When should I prescribe naloxone to a patient on a low opioid dose?
If the patient has a recent non‑fatal overdose, concurrent benzodiazepine use, or a documented substance‑use disorder, most guidelines recommend prescribing naloxone regardless of the MME level.
Can pharmacists dispense naloxone without a new prescription?
Yes. As of 2023, 49 states have standing orders that allow pharmacists to provide up to 50 doses of naloxone without a separate prescription, provided the patient meets certain risk criteria.
What are the storage requirements for intranasal naloxone?
Intranasal kits are stable at room temperature (15‑30 °C) for up to two years. Keep them away from direct sunlight and moisture, and replace any kit past its expiration date.
How do I bill for naloxone under Medicaid?
Most state Medicaid programs cover naloxone under a separate benefit code with a $0‑$5 copay. Use the HCPCS code J2315 for injectable kits or J2310 for nasal spray, and note the SUPPORT Act as the payer justification.
What should I tell a patient’s family about administering naloxone?
Explain the S.L.A.M. steps, demonstrate the device, stress the importance of calling 999 after administration, and reassure them that a single dose is usually safe even if the person isn’t overdosing.
By weaving naloxone into routine opioid prescribing, clinicians turn a high‑risk treatment into a safer one. The data, the guidelines, and the real‑world stories all point to one clear message: give the antidote before the crisis hits, and you’ll save more lives.




Marilyn Pientka
October 24, 2025 AT 13:06It is incumbent upon every prescriber to internalize the ethical imperative of naloxone co‑prescribing, lest we tacitly endorse iatrogenic mortality. The epistemic burden of overlooking ≥50 MME thresholds constitutes a dereliction of fiduciary duty, exacerbating systemic harm. Utilitarian calculus dictates that integrating a rescue pharmacologic adjunct is a non‑negotiable prophylactic measure. Moreover, the jurisprudential trend toward state mandates underscores the normative expectation of universal dissemination.
Kathryn Rude
October 24, 2025 AT 14:13Honestly, this is just basic humanity in action :) we all know the stats are screaming the same thing stop overthinking and just give the kits
Jacqueline Galvan
October 24, 2025 AT 16:10Thank you for this comprehensive guide; it elucidates the practical steps clinicians must undertake. The inclusion of the CDC MME calculator streamlines risk stratification, which is essential for accurate assessment. Providing clear patient education via the S.L.A.M. framework enhances caregiver confidence and can markedly reduce response time during an overdose event. Moreover, documenting each component in the EHR satisfies both clinical and regulatory requirements. I encourage all providers to adopt this protocol to improve patient safety outcomes.
Amanda Vallery
October 24, 2025 AT 17:00Totally agree its super easy to just add a nasal spray to the script. Gotta make sure the pharmacy has it in stock.
Carla Taylor
October 24, 2025 AT 18:56love how they broke it down easy
just pull the calculator and go
no big deal
Tammy Watkins
October 24, 2025 AT 19:46In the grand tapestry of opioid stewardship, the omission of naloxone is nothing short of a tragic oversight. One must not merely acknowledge the data but act upon it with unwavering resolve. The protocol delineated herein furnishes a veritable arsenal against needless mortality. Let us, therefore, promulgate this regimen with the solemnity it rightfully commands.
Dawn Bengel
October 24, 2025 AT 21:43👊🇺🇸 It's time America stops playing second fiddle to opioid deaths. Every clinic that hesitates to prescribe naloxone is betraying its citizens. Get proactive or get left behind! 💥
Dason Avery
October 24, 2025 AT 22:33The moral calculus aligns with compassion 🌱-empowering families to intervene transforms tragedy into hope. Let us view each prescription as an ethical covenant, a promise to safeguard life. Together we can rewrite the narrative of opioid care 🙏.
HILDA GONZALEZ SARAVIA
October 25, 2025 AT 00:30One point that deserves emphasis is the role of interdisciplinary collaboration in naloxone distribution. Pharmacists, nurses, and social workers can all reinforce education and ensure kits are accessible. Additionally, regular audit of prescription patterns helps identify gaps in adherence to the guidelines. By fostering a culture of shared responsibility, we amplify the protective net for patients at risk.
Dahmir Dennis
October 25, 2025 AT 01:20Oh, what a revelation it is that we finally had to tell doctors to hand out a life‑saving antidote instead of letting the system crumble under its own negligence. The sheer brilliance of waiting until a patient has already overdosed before offering any form of rescue is, frankly, a masterclass in bureaucratic indifference. It apparently took a handful of studies, a few hundred thousand deaths, and a mountain of public outcry before policy makers decided that co‑prescribing naloxone was not just optional but mandatory. One would think that a medication capable of reversing opioid toxicity within minutes would be a staple in any responsible clinician’s toolkit, yet here we are, patting ourselves on the back for finally catching up to the year 2000. The guidelines now demand risk assessment, documentation, patient education, and a follow‑up plan, as if these steps are groundbreaking innovations rather than elementary medical practice. And let us not forget the charmingly burdensome paperwork required to satisfy state mandates, because nothing says “patient safety” like an extra checkbox on a digital form. Meanwhile, the real victims-those families who have watched loved ones slip away-are expected to thank us for the delayed reform. The CDC’s own data shows a modest reduction in emergency visits, which makes the whole effort feel like a half‑hearted band‑aid on a gaping wound. Moreover, the cost of a generic nasal spray, though relatively low, is still a barrier for many uninsured patients, highlighting the persistent inequities in our healthcare system. It is also worth noting that some clinicians still resist prescribing naloxone out of fear that it will encourage drug use, an argument as outdated as the notion that cigarettes are harmless. The truth is, providing naloxone does not promote addiction; it merely acknowledges the reality of opioid exposure and offers a safety net. The guidelines also underscore the importance of using the S.L.A.M. framework, because apparently we need an acronym to remind us to be compassionate. In the end, the success of this initiative will hinge not on the brilliance of the policy but on the willingness of providers to embrace it without prejudice. So, here’s to finally getting it right, even if it took a decade of suffering to get there. Let’s hope the next public health crisis receives the same level of proactive attention we’ve just (barely) managed.
Jordan Levine
October 25, 2025 AT 03:16🔥 This is the kind of grassroots revolution we need-no more half‑measures, full‑on naloxone deployment! 🌍 Every state that drags its feet is basically signing death warrants for its citizens. Let’s make the push loud enough that they can’t ignore it any longer. 🚀
Mary Mundane
October 25, 2025 AT 04:06Skip the drama, just prescribe naloxone.
Michelle Capes
October 25, 2025 AT 06:03I totally get how overwhelming all these guidelines can feel 😊. It’s okay to take it step by step, and remember you’re not alone in this journey. If you need a hand with the paperwork or counseling tips, just reach out-people are happy to help. Together we can make sure no family has to face a preventable loss. 🙏