Most people pick up their prescription with a small folded paper tucked inside the box - the medication guide. You might glance at it, toss it in a drawer, or even throw it out, thinking it’s just more paperwork. But that paper could save your life. It’s not filler. It’s your personal safety manual. And if you don’t know how to read it, you’re flying blind when it comes to overdose risks and what to do if something goes wrong.
Where to Find the Overdose Warning Section
Medication guides follow a strict format set by the FDA. You won’t find overdose warnings buried in paragraphs of tiny print. They’re in one place: the Overdosage section. Look for that exact heading - usually near the end of the guide, right after Warnings and Precautions and before How Supplied.
This section doesn’t say, “Don’t take too much.” It tells you exactly what happens when you do. For example, if you’re taking oxycodone, the guide will state: “Overdose may cause severe respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and in some cases, death.” That’s not vague. It’s specific. And it’s not just about symptoms - it tells you what dose levels are dangerous. For tramadol, it might say: “Single doses greater than 400 mg have been associated with seizures and serotonin syndrome.” That’s the number you need to remember.
Look for the Boxed Warning - It’s the Red Flag
Some medications come with a black border around a section at the very top of the guide. That’s called a Boxed Warning. It’s the FDA’s strongest alert. If your medication has one, it means the risk is serious enough that the government requires it to be front and center.
For example, benzodiazepines like alprazolam have a Boxed Warning that says: “Concomitant use with opioids can result in profound sedation, respiratory depression, coma, and death.” That’s not a suggestion. That’s a warning. If you’re taking both, you’re at risk - even if you’re taking each one exactly as prescribed. The guide doesn’t say “be careful.” It says death. That’s the signal to talk to your doctor, not ignore it.
What to Look for in the Antidote Section
Not every guide lists an antidote - but the ones that do are critical. Antidotes are not always obvious. Naloxone isn’t listed under “Antidote.” It’s listed under Overdosage or sometimes in the Warnings and Precautions section. Look for phrases like:
- “Naloxone may be used to reverse opioid-induced respiratory depression.”
- “Flumazenil is a competitive antagonist at benzodiazepine receptors and may be used in overdose.”
- “Activated charcoal may be administered if ingestion occurred within the last hour.”
These aren’t instructions for you to give yourself. They’re information for emergency responders - but if you know what’s listed, you can tell paramedics: “My meds list naloxone as the antidote.” That speeds up treatment. Time matters. In opioid overdoses, every minute without oxygen can cause brain damage.
Don’t Ignore the Contraindications
Contraindications aren’t just about allergies. They’re about what you can’t mix. For example, if you’re on a serotonin-norepinephrine reuptake inhibitor (SNRI) like venlafaxine, the guide will warn: “Contraindicated with MAOIs.” Why? Because mixing them can cause serotonin syndrome - a life-threatening spike in body temperature, muscle rigidity, and seizures. The guide won’t say “don’t drink alcohol.” It says what combinations are deadly.
Check this section even if you think you’re not taking anything else. Over-the-counter painkillers, herbal supplements like St. John’s Wort, or even cough syrups with dextromethorphan can interact. The guide will tell you. You just have to look.
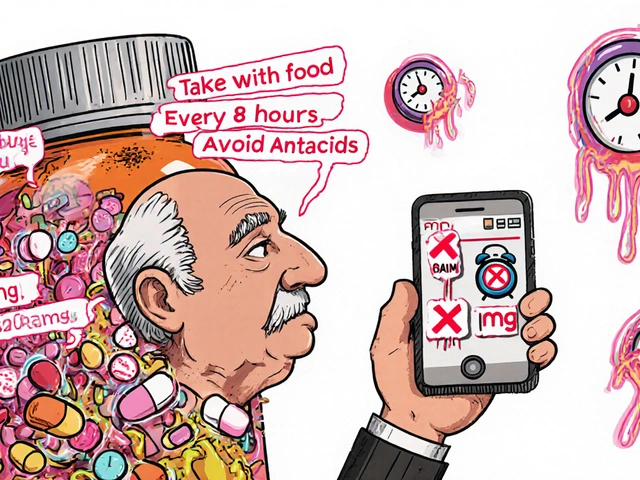
Understand the Numbers - Dose Matters
Many people think “more pills = more relief.” That’s dangerous. The guide gives you exact numbers. For instance:
- Acetaminophen: Over 7.5 grams in 24 hours can cause liver failure.
- Carbamazepine: Toxic levels start at 12 mg/L in blood - but you don’t need a lab test to know if you took 10 pills at once.
- Metoprolol: Overdose can cause dangerously slow heart rate - and the guide says doses over 200 mg have caused cardiac arrest.
You don’t need to memorize every number. But if you’re on a medication with a narrow safety margin, write down the overdose threshold and keep it in your wallet. If you ever need emergency care, that piece of paper could be the difference between life and death.
Read the Warnings About Withdrawal and Rebound Effects
Some medications don’t cause overdose in the traditional sense - but stopping them suddenly can be deadly. For example, clonidine (used for high blood pressure and ADHD) can cause sudden spikes in blood pressure if stopped abruptly. The guide will say: “Do not discontinue abruptly - taper under medical supervision.”
Similarly, antidepressants like paroxetine can cause withdrawal seizures if stopped cold. These aren’t “side effects.” They’re withdrawal reactions that mimic overdose symptoms. The guide tells you how to avoid them. If you’re thinking of stopping a medication, don’t guess - check the guide. Then talk to your doctor.
What to Do If You Suspect an Overdose
Reading the guide isn’t just about prevention - it’s about action. If you or someone else shows signs of overdose - slow breathing, unresponsiveness, blue lips, pinpoint pupils - don’t wait. Call emergency services immediately. But here’s what you can do while you wait:
- Check the medication guide for the antidote. If it says naloxone, use it. Naloxone is available without a prescription in the UK and many US states.
- If you don’t have naloxone, don’t panic. Keep the person awake and breathing. Lay them on their side - this prevents choking if they vomit.
- Bring the medication guide with you to the hospital. Paramedics and ER staff will ask what you took. The guide has the exact name, dose, and antidote. That saves time.
Don’t assume someone else knows what’s in your meds. If you’re alone, keep the guide on your phone or in your purse. If you’re caring for someone else, keep a copy in your phone notes.
Common Mistakes People Make
People skip the guide because they think:
- “My doctor explained it.” - Doctors have 10 minutes. They can’t cover every interaction.
- “I’ve taken this for years.” - Your liver changes. Your other meds change. Your risk changes.
- “It’s just a pill. How dangerous can it be?” - Acetaminophen is in 600+ products. Taking two painkillers at once can easily push you over the 4,000 mg daily limit - and you won’t feel a thing until your liver fails.
The guide doesn’t care if you’re “experienced.” It only cares about what’s in your body.
How to Make This Part of Your Routine
Make reading the guide part of your medication ritual. When you get a new prescription:
- Open the box. Take out the guide.
- Find the Overdosage section. Highlight the overdose threshold and antidote.
- Write the name of the antidote on a sticky note and stick it to your pill bottle.
- Take a photo of the guide and save it in your phone under “Medication Safety.”
- When you refill, check if the guide changed. Manufacturers update them.
It takes 90 seconds. But in a crisis, those 90 seconds could mean your life - or someone else’s.
What If the Guide Doesn’t Mention an Antidote?
Some medications don’t have a specific antidote. That doesn’t mean there’s nothing to do. It means you need to act fast. For example:
- SSRIs like sertraline - no antidote, but activated charcoal may help if taken within an hour.
- Antipsychotics like quetiapine - no antidote, but symptoms like seizures and low blood pressure need immediate IV fluids and monitoring.
If there’s no antidote listed, the guide still tells you what symptoms to watch for. That’s your early warning system. If you see them - call for help. Don’t wait for “proof.”
Why This Matters More Than Ever
More people are taking multiple medications. More are mixing prescriptions with over-the-counter drugs or supplements. And the number of accidental overdoses is rising - especially among older adults and those with chronic conditions.
The medication guide is your only direct line to the science behind your pills. It’s written by the drug manufacturer, reviewed by the FDA, and updated when new risks are found. No app, no website, no YouTube video is as reliable.
You don’t need to be a doctor to read it. You just need to look.







Emily Craig
November 26, 2025 AT 01:12Yall seriously need to stop treating these guides like junk mail I found one in my mom’s drawer last year after she almost died from mixing her blood pressure med with that herbal tea she swears is ‘all natural’ and it literally said ‘CONTRAINDICATED WITH HIBISCUS’ in bold like it was screaming at us and we just ignored it because ‘she’s been fine for years’
Josh Zubkoff
November 27, 2025 AT 12:37Look I get it the FDA wants us to read these things but let’s be real most of these guides are written by lawyers who’ve never taken a pill in their life and are trying to cover their asses so they say things like ‘may cause death’ when what they really mean is ‘if you take 40 pills at once and then jump off a bridge while on fire it might not end well’ but the point is you’re supposed to notice the pattern not the drama like why does every guide mention naloxone like it’s the hero of the story when half the people reading this don’t even know what a syringe looks like
fiona collins
November 27, 2025 AT 17:34Read the guide. Highlight the overdose threshold. Save the photo. Keep it handy. Simple. Effective. Life-saving.
Rachel Villegas
November 28, 2025 AT 02:03I’ve been on antidepressants for over a decade and I always read the guide when I refill. Last month I noticed a new warning about grapefruit interaction I’d never seen before. I called my pharmacist and they updated my med list. That’s how you stay safe.
giselle kate
November 29, 2025 AT 07:51Why are we letting big pharma dictate our health with these tiny papers when the real problem is that the government lets them charge $500 for a pill that costs 2 cents to make and then tells us to read a 10-page pamphlet instead of fixing the system you think reading about naloxone is going to fix capitalism no it’s not it’s just another distraction while they keep raising prices
Arup Kuri
November 30, 2025 AT 23:53you think this is about safety no its about control the government wants you scared so youll never question your meds they put the antidote in the guide so you think its safe to take it but what if the antidote is also controlled by them what if naloxone is only available because they want to keep you alive just long enough to keep paying for your prescription
Pallab Dasgupta
December 2, 2025 AT 23:06I used to toss these guides until my buddy OD’d on tramadol and the paramedics asked what he took and his girlfriend had no clue but I remembered reading that 400mg seizure warning so I yelled it from the ambulance and they gave him flumazenil right away and he’s alive today because of that one line I read on a Tuesday morning while eating toast
Ellen Sales
December 3, 2025 AT 01:56Reading the guide isn’t about being paranoid its about being prepared like how you check the fire extinguisher before you start a campfire you dont do it because you expect a fire you do it because you know life doesnt care if you’re busy or tired or think it’s unnecessary and when the moment comes you’ll be glad you did it not because you were smart but because you cared enough to look