Side Effect Management Assistant
Select a side effect to view management strategies
Starting or staying on a lamivudine‑zidoviedine combination can feel like walking a tightrope-one misstep and you’re hit with nausea, fatigue, or even more serious health worries. This guide walks you through the most common side effects, why they happen, and concrete steps you can take to keep them under control without stopping your life‑saving HIV treatment.
What You’re Taking: The Basics
Lamivudine is a nucleoside reverse transcriptase inhibitor (NRTI) that blocks HIV from copying its genetic material. It’s usually paired with other drugs to build a strong barrier against the virus.
Zidovudine is another NRTI that was one of the first drugs approved for HIV and works by interrupting the virus’s replication cycle. When combined, these two agents form a backbone for many once‑daily regimens.
Both drugs belong to the larger umbrella of Antiretroviral Therapy (ART) that suppresses HIV, improves immune function, and reduces the risk of transmission. The goal of ART is simple: keep your viral load undetectable and your CD4 count healthy.
Why Side Effects Happen
Even though lamivudine and zidovudine are well‑studied, they can still irritate the body’s normal processes. NRTIs interfere with the way cells make DNA, which can affect rapidly dividing cells like those in the bone marrow or digestive tract. The result? Symptoms ranging from mild nausea to more serious conditions such as anemia or lactic acidosis.
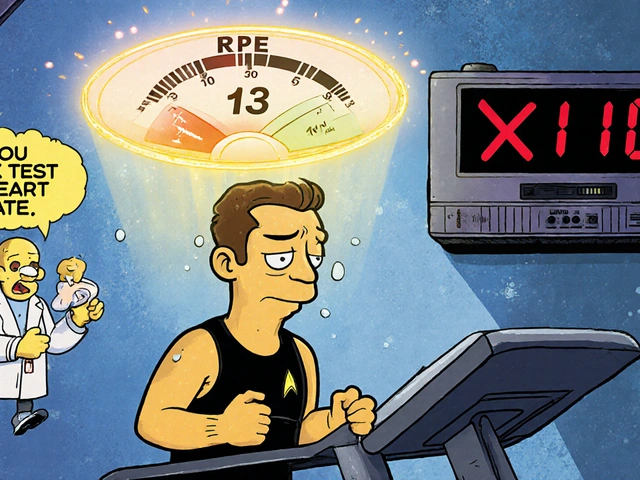
Understanding the underlying mechanism helps you predict what to watch for. For example, if the drug slows down red‑blood‑cell production, you’ll likely notice fatigue or shortness of breath-classic signs of Anemia a reduction in hemoglobin that leads to tiredness, pallor, and reduced exercise tolerance.
Common Side Effects and How to Manage Them
| Side Effect | Typical Onset | Management Strategies |
|---|---|---|
| Nausea & vomiting | First 2 weeks | Take medication with food, small frequent meals, ginger tea, anti‑emetic if needed |
| Fatigue | Variable | Assess anemia, improve sleep hygiene, moderate exercise, stay hydrated |
| Headache | First month | Hydration, over‑the‑counter acetaminophen, monitor blood pressure |
| Anemia | Weeks to months | Complete blood count monitoring, iron supplementation, consider dose adjustment with clinician |
| Lactic acidosis | Rare, months‑to‑years | Immediate medical evaluation, discontinue NRTIs, correct metabolic imbalance |
| Liver toxicity | Months | Regular liver‑function tests, avoid alcohol, discuss alternative regimens if enzymes rise |
| Drug interactions | Any time | Review all medications with pharmacist, adjust timing or switch agents |

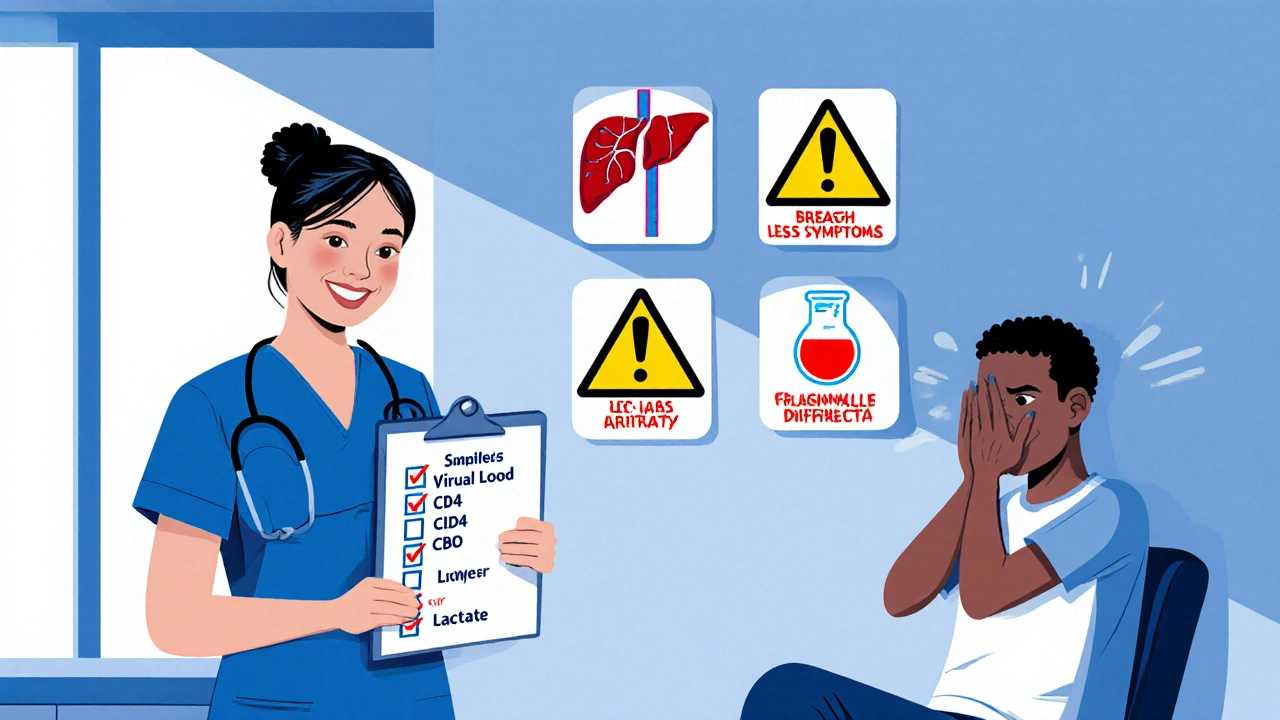
Monitoring Your Health: Lab Tests & Check‑Ins
Proactive monitoring is your safety net. Here’s what to keep on your calendar:
- Viral load: Every 3‑6 months to ensure the regimen stays effective.
- CD4 Count (CD4 Count a measure of immune system health; higher numbers mean better protection against opportunistic infections): Same interval as viral load, especially after any dose change.
- Complete blood count (CBC): Every 1‑3 months for the first six months, then quarterly. Watch for drops in hemoglobin that could signal anemia.
- Liver function tests (ALT, AST): Baseline, then at month 1, month 3, and semi‑annually.
- Lactate levels: Only if you develop unexplained muscle pain, rapid breathing, or severe nausea-signs of lactic acidosis.
Bring a written list of every supplement, over‑the‑counter drug, and prescription to each appointment. A fresh set of eyes-often a pharmacist-can catch interactions before they become problems.
When to Call the Doctor Immediately
Some symptoms aren’t just annoying; they’re red flags that need urgent attention. Call your healthcare team right away if you experience:
- Sudden, severe abdominal pain or swelling.
- Persistent vomiting that prevents you from keeping fluids down.
- Shortness of breath or chest pain at rest.
- Yellowing of the skin or eyes (jaundice).
- Unexplained rapid weight loss or extreme fatigue.
These could indicate liver toxicity, severe anemia, or Lactic Acidosis a rare but life‑threatening buildup of lactic acid in the blood, often linked to NRTI use. Prompt medical care can prevent complications.
Lifestyle Tweaks That Reduce Discomfort
Even without meds, daily habits can soften the blow:
- Stay hydrated: Aim for at least 2 L of water daily; dehydration worsens nausea and kidney stress.
- Balanced diet: Include iron‑rich foods (spinach, lentils, lean meat) to combat anemia.
- Gentle exercise: Walking or yoga improves circulation and can lessen fatigue.
- Avoid alcohol: Alcohol adds strain to the liver, especially when you’re already monitoring liver enzymes.
- Stress management: Mindfulness, deep breathing, or short breaks can reduce headache frequency.
These tweaks don’t replace medical advice, but they give your body a better chance to handle the drugs.
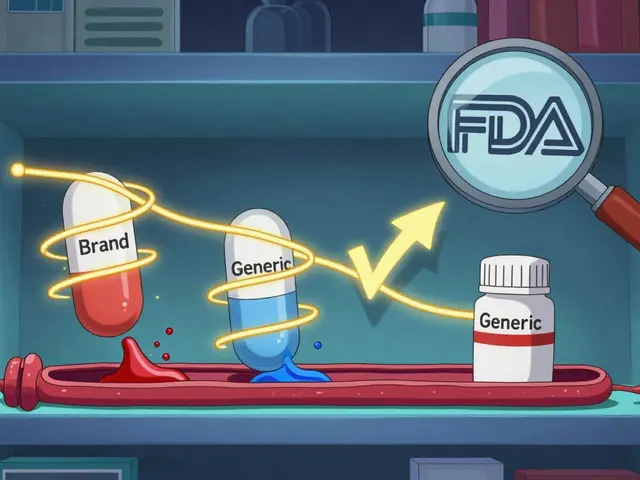
Adjusting the Regimen: When and How
If side effects linger despite your best efforts, your provider might consider dose adjustments or swapping one of the NRTIs for a newer agent like tenofovir alafenamide. The decision hinges on three factors:
- Severity of side effects: Grade 3-4 toxicities usually trigger a change.
- Virologic control: If your viral load stays undetectable, a switch is safer.
- Overall health profile: Co‑existing conditions (e.g., hepatitis B) influence which alternatives are viable.
Never switch or stop drugs on your own. A structured plan, often involving a “bridge” medication, prevents viral rebound and resistance.
Quick Reference Checklist
- Take pills with a meal or snack.
- Log any new symptoms in a notebook or app.
- Schedule lab tests: viral load, CD4, CBC, liver enzymes.
- Review all meds with your pharmacist every 6 months.
- Contact your clinic immediately for red‑flag symptoms.
Frequently Asked Questions
Can I take lamivudine‑zidovudine with over‑the‑counter medicines?
Yes, but you should always check with a pharmacist first. Some common OTC drugs-like certain antacids or herbal supplements-can alter absorption or increase toxicity. A quick medication review can keep you safe.
How long do nausea and headaches usually last?
Most people feel these symptoms for the first 1‑2 weeks. If they persist beyond a month, let your clinician know-there may be a dose tweak or a supportive medication that can help.
Is anemia from zidovudine reversible?
Often, yes. Reducing the dose or switching to a different NRTI can allow bone‑marrow recovery within a few weeks, especially when iron intake is optimized.
What signs should I watch for that indicate lactic acidosis?
Look for unexplained muscle pain, rapid breathing, abdominal discomfort, and a feeling of extreme weakness. If any of these appear, seek emergency care right away.
Can lifestyle changes really reduce side effects?
Yes. Hydration, a balanced iron‑rich diet, and regular low‑impact exercise have been shown in multiple cohort studies to lower the incidence of fatigue and anemia in patients on NRTIs.
Managing side effects is a partnership-your body, your meds, and your care team all play a role. With the right monitoring, a few daily habits, and quick action when warning signs appear, you can stay on lamivudine‑zidovudine and keep your HIV under control.




James Mali
October 18, 2025 AT 14:46The anti‑nausea tip to eat with food is common sense 😊.
Janet Morales
October 22, 2025 AT 14:46Starting on lamivudine‑zidovudine feels like signing a pact with a volatile beast. You think you’re just swallowing pills, but the body reacts like a rebellious teenager. Nausea bursts in the first two weeks like an unwelcome guest that refuses to leave. Headaches follow, thumping on the temples as if a drum line marched inside your skull. Fatigue creeps in, turning simple chores into Everest climbs. Anemia lurks in the blood, stealing oxygen and leaving you pale and winded. Lactic acidosis is the silent assassin that hides behind muscle pain and rapid breathing. The guide says hydrate, but “hydrate” feels like a cruel joke when you’re constantly vomiting. Iron‑rich foods are suggested, yet the nausea makes you throw up everything you eat. Exercise is recommended, but the fatigue makes the idea of a walk sound like torture. Doctors want regular labs, but waiting weeks for results feels like being trapped in a waiting room of dread. The side‑effect table looks tidy, but each entry is a potential nightmare. Switching drugs is touted as a solution, yet the fear of viral rebound lurks like a shadow. You’re told not to stop meds on your own, but the discomfort can feel like a prison sentence. In the end, navigating this regimen is a daily battle of willpower, medical advice, and gut‑level survival instincts.
Albert Fernàndez Chacón
October 26, 2025 AT 13:46Keeping an eye on your CBC and liver enzymes every few months is a solid habit. It helps catch anemia or toxicity before they become big problems. Pair that with a balanced diet-spinach, lentils, and lean meat boost iron. Staying hydrated also eases nausea and supports kidney function. If you notice fatigue creeping up, chat with your clinician about a possible dose tweak.
Drew Waggoner
October 30, 2025 AT 13:46Side effects can feel like a personal attack, especially when the nausea won’t quit. Listening to your body and reporting changes early is the only way to stay ahead.
Liberty Moneybomb
November 3, 2025 AT 13:46What most guides hide is the data that pharma companies keep under lock‑and‑key, saying “manage side effects” while they profit from our suffering. They push these combos because they own the patents, not because they’re the safest. You’re basically a lab rat in a corporate experiment, and the “quick reference” checklist is just a PR stunt.
Alex Lineses
November 7, 2025 AT 13:46Great points! For anyone struggling with anemia, consider adding a ferrous sulfate supplement and checking vitamin B12 levels-it can make a noticeable difference. Also, set reminders for your lab appointments; a phone alarm works better than relying on memory. If you ever feel the fatigue is out of proportion, request a dose review with your provider; many clinicians are happy to adjust the regimen for tolerability.
Brian Van Horne
November 11, 2025 AT 13:46In sum, adherence paired with vigilant monitoring constitutes the cornerstone of successful therapy.
Poornima Ganesan
November 15, 2025 AT 13:46Honestly, if you’re still relying on outdated zidovudine‑based regimens, you’re ignoring a decade of advances in antiretroviral therapy. Modern tenofovir‑based combinations offer superior tolerability and lower hematologic toxicity, and most guidelines now recommend them as first‑line. Clinging to legacy drugs not only jeopardizes your health but also fuels unnecessary side‑effect burden.
Emma Williams
November 19, 2025 AT 13:46Staying hydrated really does help with nausea and fatigue
Stephanie Zaragoza
November 23, 2025 AT 13:46While it is commendable that patients maintain a diligent medication schedule, one must also recognize that the concomitant ingestion of high‑fat meals can exacerbate gastrointestinal discomfort, thereby diminishing overall adherence, and consequently, therapeutic efficacy.
Rajesh Singh
November 27, 2025 AT 13:46We have a responsibility to treat our bodies with respect; ignoring the warning signs of anemia or lactic acidosis is tantamount to neglecting a neighbor in distress. When you feel inexplicable weakness, speak up-silence only empowers the disease.
Mike Hamilton
December 1, 2025 AT 13:46i think its importent to check labs regurarly dont wait until you feel sicks. simple diet and water help alot.
Matthew Miller
December 5, 2025 AT 13:46Push through the first tough weeks! Keep a symptom journal, celebrate each day you stay on track, and remember: every dose taken brings you closer to an undetectable viral load. You’ve got this!
Norman Adams
December 9, 2025 AT 13:46Oh, because journaling your misery is the groundbreaking solution everyone’s been waiting for-how ever‑so‑innovative.