Take your antibiotic with your antacid. It seems harmless-maybe even helpful. You’ve got heartburn, you’ve got an infection, and you just want to feel better. But if you’re taking antibiotics like ciprofloxacin or doxycycline with an antacid, you might be making your infection worse.
Why Antacids Can Ruin Your Antibiotic
Antacids don’t just neutralize stomach acid-they also bind to certain antibiotics and stop them from being absorbed. This isn’t a minor issue. When you take an antacid at the same time as a fluoroquinolone like ciprofloxacin or a tetracycline like doxycycline, the antibiotic’s effectiveness can drop by up to 90%. That means the drug never reaches the level needed to kill the bacteria. Instead of clearing your infection, you’re left with a stubborn one that might come back stronger.This happens because antacids contain aluminum, magnesium, or calcium. These minerals latch onto the antibiotic molecules, forming a compound your body can’t absorb. Think of it like putting a lock on the antibiotic-your gut can’t open it. At the same time, antacids raise the pH in your stomach. Some antibiotics need acid to dissolve properly. If the environment becomes too basic, they just sit there, unchanged and useless.
Which Antibiotics Are Most Affected?
Not all antibiotics are equally vulnerable. The ones most at risk are those that rely on absorption in the upper intestine and are sensitive to metal ions or pH changes.- Fluoroquinolones (ciprofloxacin, levofloxacin): These are the most affected. Studies show up to 90% less absorption when taken with antacids. A 2021 FDA analysis found that patients who took ciprofloxacin within 2 hours of an antacid had a 22% higher chance of treatment failure for urinary tract infections.
- Tetracyclines (doxycycline, tetracycline): These bind tightly to calcium and magnesium. Absorption drops by 50-70%. That’s why acne patients on doxycycline often don’t improve-they’re taking it with their morning Tums.
- Other antibiotics: Some, like amoxicillin or azithromycin, are less affected. But even they can lose 15-20% of their effectiveness if taken with antacids. It’s not zero risk-it’s just lower.
- Safe options: Metronidazole and some penicillins show no significant interaction. If you’re on one of these, you can skip the timing drama.
How Far Apart Should You Take Them?
Timing isn’t guesswork. It’s science. And the separation window depends on the antibiotic.The gold standard recommended by the FDA, NHS, and Cleveland Clinic is this:
- For ciprofloxacin or other fluoroquinolones: Wait 4 hours after taking an antacid, or take the antibiotic 2 hours before the antacid.
- For doxycycline or other tetracyclines: Wait 2-3 hours after the antacid, or take the antibiotic 1-2 hours before.
- For amoxicillin or azithromycin: A 1-hour gap is usually enough. Still, better safe than sorry.
Why the difference? Fluoroquinolones bind more tightly to metals and take longer to clear from the gut. Tetracyclines are less stubborn but still need space. The 4-hour window for ciprofloxacin isn’t arbitrary-it’s based on how long it takes the antacid’s minerals to be flushed out of the absorption zone.
Real Cases: What Happens When People Ignore Timing
On Reddit, a patient wrote: “I took ciprofloxacin for a UTI with my Tums. Two days later, I was back in the ER. My doctor asked if I took them together. I said yes. He said that’s why it didn’t work.”That’s not rare. A 2023 Drugs.com survey of 1,247 patients found that 68% who experienced treatment failure later realized they’d taken their antibiotic and antacid together. Once they separated the doses, their symptoms improved within days.
Another case: A 72-year-old woman on doxycycline for a lung infection was also taking calcium-based antacids for acid reflux. Her infection didn’t clear. Her pharmacist noticed the timing conflict, adjusted her schedule, and within two weeks, she was symptom-free. No new prescription. Just better timing.
What If You Need Antacids All Day?
Some people need antacids frequently-after every meal, even at bedtime. That makes sticking to a 4-hour gap impossible.Here’s what doctors do in real life:
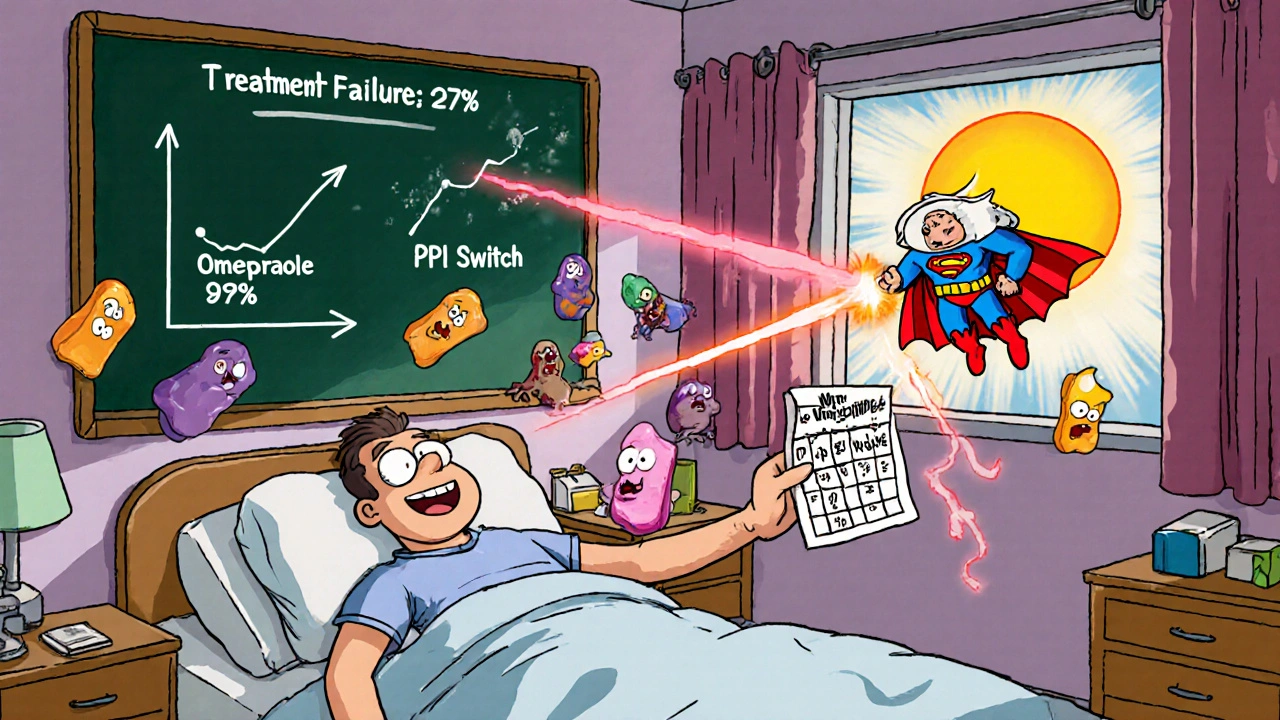
- Switch to H2 blockers like famotidine (Pepcid) or ranitidine (though ranitidine is largely phased out). These reduce acid production without binding to antibiotics.
- Use proton pump inhibitors like omeprazole or pantoprazole. They’re longer-lasting and don’t interfere with antibiotic absorption.
- Limit antacid use to only when absolutely necessary. If you’re taking antacids daily, you might have a condition like GERD that needs a different long-term solution.
A 2023 study in the Journal of Clinical Pharmacy and Therapeutics showed that switching from antacids to PPIs in patients on antibiotics dropped treatment failure rates from 27% to just 9%. That’s a 67% improvement-just by changing the acid reducer.
How to Remember the Timing
The hardest part isn’t knowing the rule-it’s remembering it.Most people don’t have a pharmacy assistant hovering over them. Here’s what works:
- Use a medication app: MyMedSchedule, Medisafe, or even Apple Health can be set to alert you when to take each pill. Some even show a visual timeline: “Antibiotic at 8 AM. Antacid not until 12 PM.”
- Write it down: Stick a note on your bathroom mirror: “Cipro at 8 AM. Tums after lunch at 1 PM.”
- Ask your pharmacist: They’re trained to catch these interactions. If you’re picking up both meds, ask: “Should I take these at different times?” Most will give you a printed schedule.
- Use visual cues: Take your antibiotic with breakfast. Take your antacid with dinner. That’s a simple, reliable rhythm.
A Mayo Clinic study found that patients who got a printed timing chart reduced their dosing errors by 37%. Simple tools make a big difference.
What About Newer Antibiotics?
In May 2023, the FDA approved a new version of ciprofloxacin called Cipro XR-24. It’s designed to be absorbed lower in the gut, where antacids have less effect. In trials, it showed only an 8% drop in absorption when taken with antacids-compared to 90% for the old version.This is a game-changer. But it’s not widely available yet, and it costs more. For now, most people are still on the older forms. Until the new version becomes standard, timing still matters.
What’s the Bigger Picture?
This isn’t just about one pill not working. Improper timing contributes to antibiotic resistance. When you don’t get enough of the drug into your system, bacteria survive. They adapt. They become stronger. The CDC estimates that 15% of new fluoroquinolone resistance cases trace back to subtherapeutic levels caused by antacid interactions.And the cost? The U.S. spends $1.2 billion a year treating infections that failed because of simple dosing errors. That’s $1.2 billion in extra doctor visits, lab tests, and hospital stays-all preventable.
Bottom Line: Do This Today
If you’re taking an antibiotic and an antacid:- Check the name of your antibiotic. Is it ciprofloxacin, levofloxacin, doxycycline, or tetracycline? If yes, timing is critical.
- Don’t take them together. Wait at least 2 hours before or after.
- If you’re on ciprofloxacin, wait 4 hours after the antacid.
- If you need acid relief often, ask your doctor about switching to famotidine or omeprazole.
- Use an app or write down your schedule. Don’t rely on memory.
- When you pick up your prescription, ask your pharmacist: “Do I need to separate this from my antacid?”
This isn’t complicated. It’s not about being perfect. It’s about being smart enough to avoid a mistake that could cost you weeks of illness-and maybe even your health.
Can I take antacids with amoxicillin?
Yes, but not at the same time. Amoxicillin is less affected than ciprofloxacin or doxycycline, but studies show it can still lose 15-20% of its absorption if taken with antacids. To be safe, wait at least 1 hour between doses. If you’re taking amoxicillin three times a day, space the antacid for after your last dose.
What if I accidentally took them together?
If it was a one-time mistake, don’t panic. Skip your next dose of the antibiotic and restart your schedule with proper timing. Don’t double up. If you’re on a short course (like 5-7 days) and you’re already halfway through, you might still be okay-but monitor for symptoms. If your infection isn’t improving after 48 hours, contact your doctor. If you’re on a long course or have a serious infection (like pneumonia or a UTI), call your doctor immediately.
Do all antacids cause this interaction?
No. Only antacids with aluminum, magnesium, or calcium cause this problem. Common brands like Tums (calcium carbonate), Maalox (aluminum/magnesium), and Mylanta (aluminum/magnesium) all interfere. Antacids with sodium bicarbonate (like Alka-Seltzer) are less likely to bind to antibiotics, but they’re not recommended for regular use due to high sodium content. Always check the active ingredients on the label.
Can I take antacids at bedtime if I take my antibiotic in the morning?
Yes, if you’re taking your antibiotic in the morning and your antacid at night, you’re likely fine. A 12-hour gap is more than enough for even the most sensitive antibiotics like ciprofloxacin. The key is avoiding overlap. If you take your antibiotic at 8 AM and your antacid at 10 PM, you’re safe. But if you take your antibiotic at 8 PM and your antacid at 10 PM, that’s a problem.
Are there any antibiotics that don’t interact with antacids?
Yes. Metronidazole (Flagyl), clindamycin, and most penicillins (like amoxicillin and ampicillin) have minimal to no interaction with antacids. Azithromycin (Zithromax) also has very low risk. But always confirm with your pharmacist. Even low-risk drugs can have exceptions depending on your health or other medications.
Why do some doctors say it’s not a big deal?
Some experts argue that for mild infections or healthy patients, a 15-20% drop in antibiotic levels might not matter. But for serious infections-like pneumonia, kidney infections, or in elderly or immunocompromised patients-that small drop can mean the difference between recovery and complications. The FDA and CDC treat this as a serious risk because of the scale: millions of people take these drugs together. Even a small failure rate adds up to thousands of avoidable hospitalizations.
Can I use natural remedies like ginger or baking soda instead of antacids?
Baking soda (sodium bicarbonate) is an antacid and can still interfere with some antibiotics, though less than aluminum or calcium-based ones. Ginger may help with nausea, but it doesn’t neutralize stomach acid. If you’re trying to avoid antacids entirely, try eating smaller meals, avoiding spicy or fatty foods, and staying upright after eating. If heartburn is chronic, talk to your doctor about PPIs or H2 blockers-they’re safer long-term and won’t mess with your antibiotics.




Curtis Ryan
November 29, 2025 AT 18:40Bro this saved my life. Took cipro with Tums by accident and woke up feeling like a zombie. Read this, spaced it out, and boom - infection gone in 3 days. You’re not crazy for caring about timing - you’re smart.
PS: I still typo everything but this? I printed it and taped it to my pillbox.
Rajiv Vyas
November 30, 2025 AT 11:39LOL so now the FDA is telling us how to live? Next they’ll ban breathing near antibiotics. I take mine with milk and antacid and I’m still alive. Maybe the real problem is Big Pharma wants you to buy more pills because yours didn’t work.
Astro Service
November 30, 2025 AT 21:26Why do we even listen to this science stuff? We used to just take pills and pray. Now we got charts and apps and 4-hour windows. This is why America’s getting weak. Back in my day we took everything together and still beat the infection. Now we’re all scared of a Tums.
DENIS GOLD
December 2, 2025 AT 04:21Wow. So now I need an app to tell me when to take my medicine? Next they’ll make me wear a badge that says ‘I Follow Guidelines.’ What’s next? Antibiotics with a QR code? 🤡
Ifeoma Ezeokoli
December 3, 2025 AT 09:09My grandma in Nigeria takes amoxicillin with pap and antacid every morning - and she’s 82 and still gardening. Maybe science doesn’t always fit real life? Not everyone has apps or fancy pills. Sometimes love and patience heal more than timing charts. 🌿
Daniel Rod
December 4, 2025 AT 02:18Just... wow. 🤯 This is one of those posts that makes you pause and think - we’re so busy trying to fix our bodies, we forget how fragile the system is. That 90% absorption drop? That’s not a statistic. That’s someone’s relapse. That’s another round of antibiotics. That’s resistance building in the shadows. Thank you for writing this like a human, not a textbook. 🙏
gina rodriguez
December 4, 2025 AT 17:40So helpful! I just started doxycycline and was wondering why my heartburn was acting up. I’ll switch to Pepcid tonight. Small change, big difference. Thanks for the clear timeline - I’m printing this out too. 💪
Sue Barnes
December 6, 2025 AT 14:40If you’re taking antacids daily, you’re doing something wrong. Stop treating symptoms and fix the root cause. No one needs to be popping Tums like candy. Eat less junk, stop lying down after meals, and maybe your doctor won’t have to prescribe you antibiotics in the first place.
jobin joshua
December 7, 2025 AT 21:49Wait so if I take cipro at 8am and antacid at 8pm - I’m good? 😅 I’ve been doing that for weeks. Thought I was being careful. Guess I’m not dumb after all. 🙌
Andrea Jones
December 8, 2025 AT 11:30Okay but why is Cipro XR-24 not on every pharmacy shelf yet? If it’s 92% effective with antacids, why are we still making people memorize 4-hour windows? This feels like a corporate delay. Someone’s making money off the confusion.
Justina Maynard
December 9, 2025 AT 19:12Let’s be real - the real villain here isn’t the antacid. It’s the fact that we’re handed prescriptions like they’re vending machine snacks. No consultation. No timing instructions. Just ‘take this twice a day.’ If your pharmacist doesn’t explain drug interactions, you’re not getting care - you’re getting a transaction.
Evelyn Salazar Garcia
December 10, 2025 AT 04:06Too much info. I’ll just skip the antacid.
Clay Johnson
December 11, 2025 AT 11:10Timing is a human construct. The body doesn’t care about clocks. It cares about chemistry. The real issue is systemic - we treat symptoms like enemies instead of signals. The antacid isn’t the problem. The fear of discomfort is.
Jermaine Jordan
December 12, 2025 AT 22:44As a medical educator, I can confirm: this is one of the most under-taught interactions in pharmacy school. Students forget it. Nurses forget it. Even some doctors assume it’s ‘not a big deal.’ But the data? It’s brutal. This post should be mandatory reading for every patient on antibiotics. Well done.