When you pick up a prescription at the pharmacy, there’s a good chance you’re getting a generic drug. About 90% of all prescriptions filled in the U.S. are for generics. But do they really work the same as the brand-name version you’ve heard of? The answer isn’t guesswork-it’s science, enforced by the FDA with some of the strictest standards in the world.
Same Active Ingredient, Same Effect
Generic drugs aren’t copies or knockoffs. They’re required by law to contain the exact same active ingredient as the brand-name drug. That means if your brand-name pill has 20 mg of atorvastatin, the generic has 20 mg of atorvastatin-no more, no less. The FDA doesn’t allow any variation in the medicine that actually treats your condition. This isn’t just a guideline; it’s a legal requirement under the Hatch-Waxman Act of 1984.How the FDA Proves They Work the Same
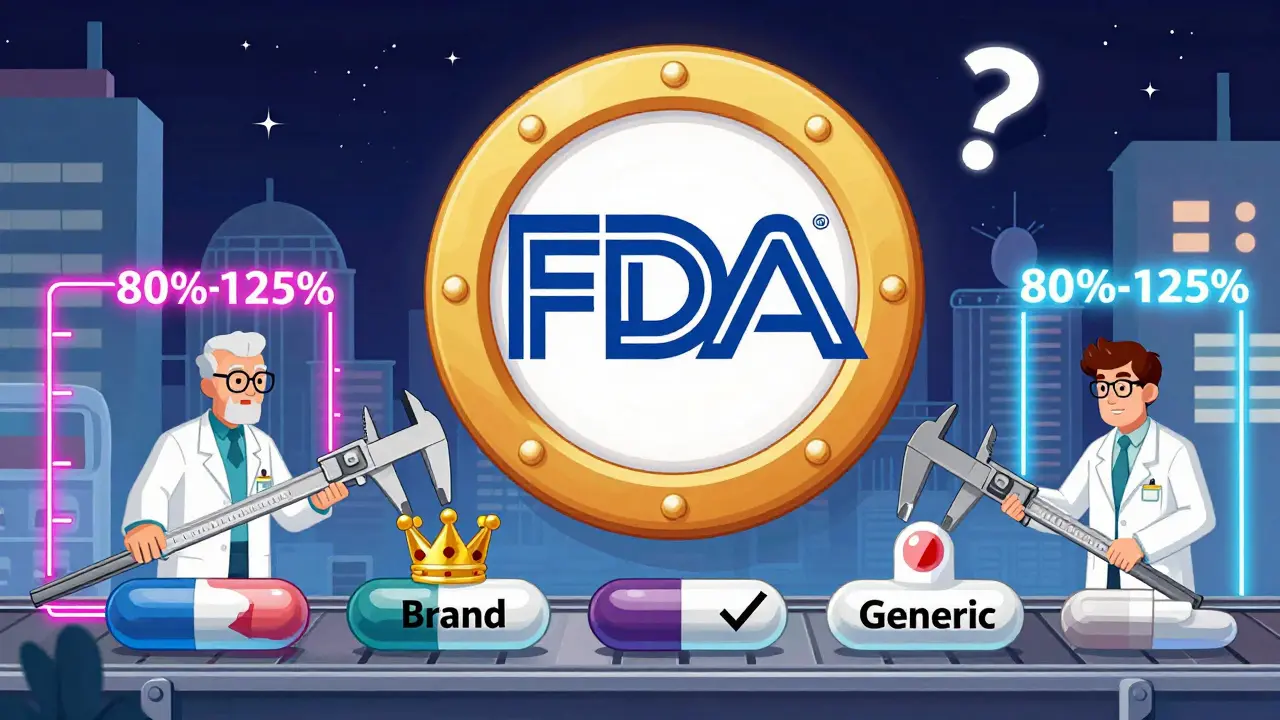
The biggest question isn’t just about ingredients-it’s about how your body absorbs them. That’s where bioequivalence comes in. To get approved, a generic drug must show it delivers the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. The FDA uses a precise scientific test: it compares the area under the curve (AUC) and the maximum concentration (Cmax) of the drug in the blood. For a generic to pass, these numbers must fall within 80% to 125% of the brand-name drug’s values. That’s not a broad range-it’s a tight window. The 90% confidence interval of the geometric mean must stay inside those bounds. This is measured in clinical studies with 24 to 36 healthy volunteers, often done in a crossover design where participants take both versions at different times. The FDA doesn’t rely on guesswork. It requires manufacturers to submit detailed reports showing every step of the testing, including statistical analysis. For complex drugs like inhalers or topical creams, the requirements are even stricter. In 2019, the FDA created a special list for narrow therapeutic index drugs-medications like warfarin or levothyroxine-where tiny differences can matter. For these, the acceptable range was tightened to 90% to 111% to ensure safety.More Than Just the Active Ingredient
It’s not just about what’s in the pill-it’s about how it’s made. The generic must match the brand in dosage form (tablet, capsule, liquid), strength, and route of administration. If the brand is an extended-release tablet, the generic must be too. The FDA requires manufacturers to prove they can make each batch consistently, with content uniformity within 85% to 115% of the labeled amount. Inactive ingredients-like fillers, dyes, or preservatives-can be different. But they’re not random. The FDA maintains an Inactive Ingredient Database that lists safe limits for over 500 excipients across 80 delivery methods. If a manufacturer wants to use something new, they have to prove it’s safe. This isn’t a loophole-it’s a safety net.
The Approval Process: ANDA vs. NDA
Brand-name drugs go through a New Drug Application (NDA), which takes years and costs hundreds of millions. It includes full animal and human trials to prove safety and effectiveness. Generic manufacturers don’t repeat that. Instead, they file an Abbreviated New Drug Application (ANDA). The FDA already knows the brand works. The ANDA just proves the generic matches it. This saves time and money, but it doesn’t mean less scrutiny. The FDA reviews every ANDA with the same rigor. In 2022, the agency approved 777 ANDAs. But nearly one-third of initial submissions were rejected outright-called Refuse-to-File letters-because they were missing critical data. The most common reasons? Inadequate bioequivalence studies (28%), manufacturing flaws (22%), and labeling errors (18%). Manufacturers must also prove their production facilities meet Current Good Manufacturing Practices (cGMP). The FDA inspects every plant-whether it’s in the U.S., India, or China-before approving a generic. If a facility fails inspection, the application is delayed. In 2022, 21% of complete response letters cited manufacturing issues.Real-World Evidence: Do Generics Actually Work?
The FDA doesn’t stop at approval. It keeps watching. The Adverse Event Reporting System (FAERS) shows that the number of reported side effects per million prescriptions is nearly identical between generics and brands: 1.7 for generics, 1.6 for brand-name drugs. A 2023 analysis of 15 million patient records by IQVIA found no meaningful difference in clinical outcomes between brand and generic versions of 20 common drugs, including metformin and atorvastatin. In fact, patients were 3.2% more likely to stick with their treatment when using generics-because they cost less. Some patients report feeling different after switching. A 2021 survey found 12% of patients said they noticed a change in effectiveness. But when doctors checked lab results and clinical markers, those differences rarely held up. The FDA attributes most of these reports to placebo effects or changes in pill appearance, not actual drug performance.
Who Makes Generics and How Much Does It Cost?
Developing a generic isn’t cheap. A typical ANDA costs between $1.5 million and $3 million. For complex products-like inhalers or injectable emulsions-it can hit $25 million. The paperwork is massive: 30,000 to 50,000 pages, organized in strict global formats. The bioequivalence section alone can be 5,000 to 10,000 pages of raw data. Teva, Viatris, and Sandoz dominate the market, but over half of all generic approvals go to smaller companies. The FDA actively encourages competition to prevent shortages. In 2017, it launched the Generic Drug Competition Action Plan to speed up approvals for drugs with few manufacturers.What’s Changing Now?
The FDA is preparing for a wave of new generics. Over $260 billion in brand-name drug sales will lose patent protection between 2024 and 2028. To handle the surge, the agency updated its user fee program (GDUFA III) in 2023, allocating $1.1 billion through 2027 to cut review times to 8 months for standard applications and 6 months for priority ones. New guidance is being issued for complex generics-like biosimilars, which are generic versions of biologic drugs. The first 15 product-specific guidances for these are due in early 2024. The FDA is also expanding its Real-Time Oncology Review program to include cancer generics, cutting approval times by 30%. The first under this program, a generic version of capecitabine, was approved in February 2024-seven months faster than usual.Why This Matters
Generic drugs save the U.S. healthcare system about $313 billion a year. Without them, many people wouldn’t be able to afford their medications. The FDA’s system ensures that cost savings don’t come at the cost of safety or effectiveness. Every generic you take has passed the same science-based tests as the brand. It’s not magic. It’s regulation, transparency, and decades of scientific rigor.Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence-meaning they deliver the same amount of medicine into your bloodstream at the same rate. Clinical studies and real-world data show no meaningful difference in effectiveness for the vast majority of drugs.
Why do some people say generics don’t work as well?
Some patients report feeling different after switching, often due to changes in pill size, color, or inactive ingredients. For most drugs, these differences are psychological or unrelated to the medicine’s effect. However, for narrow therapeutic index drugs like warfarin or levothyroxine, the FDA applies stricter bioequivalence standards. Even then, studies show clinical outcomes remain consistent when monitored properly.
Does the FDA inspect generic drug factories?
Yes. The FDA inspects every manufacturing facility-whether in the U.S. or overseas-before approving a generic drug. These inspections check for compliance with Current Good Manufacturing Practices (cGMP). In 2022, 21% of approval delays were due to manufacturing issues found during inspections. The FDA does not allow any facility with serious violations to produce generics.
Can a generic drug have different inactive ingredients?
Yes. Generic manufacturers can use different fillers, dyes, or preservatives, as long as they’re listed in the FDA’s Inactive Ingredient Database and are safe at the levels used. These changes don’t affect how the medicine works. But if a patient has an allergy to a specific ingredient (like a dye), they should check the label or ask their pharmacist.
How long does it take for the FDA to approve a generic drug?
The standard review time is 10 months, but it can take longer if the application is incomplete or if manufacturing issues arise. In 2022, the FDA met its goal of approving 91.3% of standard ANDAs within 10 months. For complex drugs or those with patent challenges, the process can extend by 6-12 months. The FDA is working to reduce this to 8 months for standard applications by 2027 under GDUFA III.
Are generics cheaper because they’re lower quality?
No. Generics are cheaper because they don’t repeat expensive clinical trials. The brand-name company already paid for those. Generic manufacturers only need to prove their product matches the original. The FDA’s standards for quality, safety, and effectiveness are identical for both. The cost difference comes from competition and lower marketing expenses-not lower quality.





Juan Reibelo
January 24, 2026 AT 01:59Wow, this is actually one of the most thorough breakdowns of generic drug regulation I’ve ever seen. The 80%-125% bioequivalence window? That’s tighter than most people realize. And the fact they test with 24-36 volunteers in crossover designs? That’s solid science. I used to think generics were just cheaper knockoffs-now I get why they’re trusted globally.
Darren Links
January 25, 2026 AT 02:15Yeah right, like the FDA actually gives a damn about quality. They approve generics from factories in India that get shut down every other year for faking data. This whole system is a joke. We’re just letting foreign labs cut corners so we can save a few bucks on pills. Meanwhile, real Americans pay for the consequences.
Kevin Waters
January 25, 2026 AT 22:50Actually, Darren, that’s a common misconception. The FDA inspects every single manufacturing plant-U.S., India, China, you name it-before approval. And if a facility fails inspection, the application gets rejected. In 2022, over 20% of rejections were due to manufacturing issues. The system’s not perfect, but it’s not broken either. Real data > fear.
Himanshu Singh
January 27, 2026 AT 03:11Beautiful breakdown 😊
Science doesn't lie. When your body absorbs the same amount of medicine at the same rate, it doesn't matter if the pill is blue or white. I’ve been on generic metformin for 8 years. My A1C? Stable. My wallet? Happy. 🙌
Jamie Hooper
January 27, 2026 AT 04:22so like… the fda just says ‘yep this generic is fine’ and we’re supposed to trust it? lol
my cousin switched to generic lisinopril and now she’s dizzy all day. coincidence? i think not.
Husain Atther
January 28, 2026 AT 06:11It's worth noting that the FDA's standards for generics are among the most rigorous in the world. Countries without similar oversight often have inconsistent quality. The fact that over 90% of U.S. prescriptions are generics speaks to both public trust and regulatory integrity. Cost efficiency without compromise is the ideal.
Helen Leite
January 30, 2026 AT 05:40EVERYONE KNOWS THE FDA IS IN BED WITH BIG PHARMA. THEY LET THE SAME COMPANIES MAKE BRAND AND GENERIC. THEY’RE JUST MAKING YOU THINK IT’S SAFE. 😈💊
Marlon Mentolaroc
January 31, 2026 AT 04:10Let’s be real-this whole post is just corporate propaganda. The FDA approved 777 ANDAs in 2022? That’s 777 opportunities for corner-cutting. And don’t get me started on the 12% of patients who report feeling different. That’s not placebo-that’s pharmacokinetic variance they’re ignoring because it’s inconvenient. Also, why are 21% of approvals delayed for manufacturing? Hmm.
Gina Beard
February 1, 2026 AT 04:31Trust is a luxury. Science is a process. Both require proof.
Don Foster
February 1, 2026 AT 06:58Anyone who still doubts generics clearly never took pharmacology. The Hatch-Waxman Act was genius. Bioequivalence isn’t a suggestion-it’s a statistical mandate. The 90% CI requirement? That’s not guesswork, that’s math. And the fact you think inactive ingredients matter? That’s why people don’t understand science.
siva lingam
February 2, 2026 AT 02:34so the fda says its all good and we just gotta believe them? cool story bro