When you pick up a prescription, you might not think about the legal rules behind whether you get the brand-name drug or a cheaper generic version. But those rules are different in every state-and they can affect your health, your wallet, and even your trust in the pharmacy. In some places, the pharmacist swaps the brand for a generic automatically. In others, they have to ask you first. In a few, they can’t substitute at all for certain drugs, no matter how much money you save. This isn’t just bureaucracy. It’s a patchwork of laws that shape how millions of Americans get their medicines every day.
Why Do State Laws on Generic Substitution Even Exist?
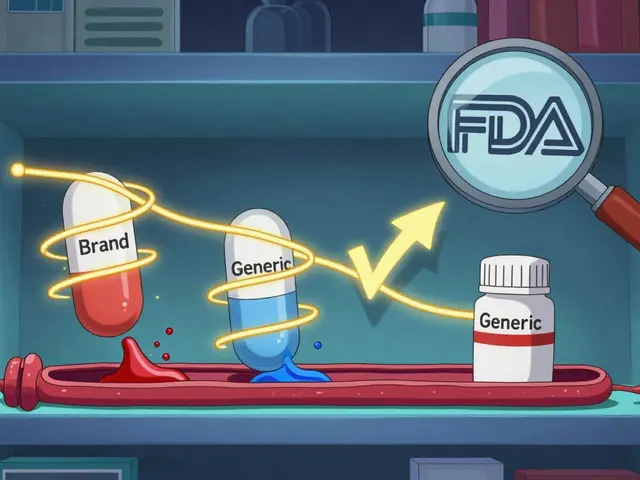
The push for generic substitution started in the 1980s after the federal Hatch-Waxman Act made it easier for drug companies to get generic versions approved. The goal was simple: lower costs without sacrificing safety. Generic drugs are chemically identical to brand-name drugs and must meet the same FDA standards. But states didn’t want to leave it up to pharmacies to decide. So each one wrote its own rules.
Today, 92.5% of all prescriptions filled in the U.S. are for generics. That’s $313 billion saved every year. But how those generics get into your hands? That depends entirely on where you live.
Mandatory vs. Permissive: Who Decides?
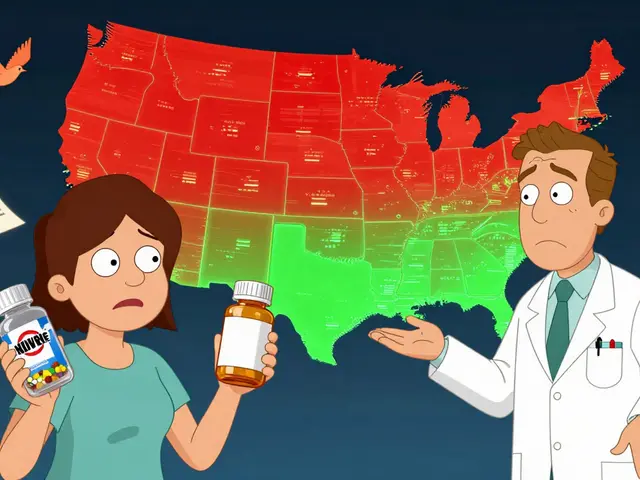
There are two main models for how pharmacists handle substitutions. In 22 states, substitution is mandatory. That means if a generic is available and the prescriber hasn’t said "dispense as written," the pharmacist must switch it. They don’t need your permission. In the other 28 states and Washington, D.C., substitution is permissive. The pharmacist can offer the generic, but they can’t force it. You have to say yes.
That difference matters. A 2018 study found that states with mandatory substitution had 12.3% higher generic fill rates for statins-drugs like atorvastatin used to lower cholesterol. That’s not just savings. It’s better access. In places like Louisiana, where laws are most favorable to substitution, patients are more likely to get the cheaper version and stick with their treatment. In Hawaii, where rules are the strictest, pharmacists need both the doctor’s and the patient’s approval to switch even common drugs like antiepileptics.
Presumed Consent vs. Explicit Consent: Do You Have to Say Something?
Even within permissive states, the rules get more complicated. Thirty-two states use presumed consent. That means if you don’t say anything, the pharmacist assumes you’re okay with the generic. Eighteen states require explicit consent. You have to actively say, "Yes, give me the generic." In New York, for example, pharmacists must ask every patient. In New Jersey, they can just swap it unless you object.
This creates real confusion. People who live near state borders often get different treatment depending on where they fill their prescription. One Reddit user, a pharmacist in New York, shared that patients from New Jersey are confused when they’re asked for permission-because back home, they never were. It’s not just a paperwork issue. It’s a trust issue. If you don’t understand why the pill looks different this time, you might think something went wrong.

What Drugs Can’t Be Substituted?
Not all drugs are treated the same. The FDA says most generics are interchangeable. But for drugs with a narrow therapeutic index (NTI), even tiny differences can matter. These are drugs where the difference between a helpful dose and a dangerous one is very small. Think warfarin (a blood thinner), levothyroxine (for thyroid problems), and some seizure medications.
Fifteen states have extra rules for these. Kentucky, for example, bans substitution for digitalis glycosides and antiepileptic drugs. Minnesota had documented cases where patients on warfarin had bad reactions after switching to a generic-even though the FDA rated it equivalent. The FDA itself admits that some patients may feel different on a generic, even if lab tests say they shouldn’t.
That’s why 41% of cancer patients surveyed by the Life Raft Group in 2023 said they were worried about substitution for NTI drugs. Many doctors now write "dispense as written" on prescriptions for these meds, especially for patients with chronic conditions.
Biosimilars: The New Frontier
It’s not just small-molecule generics anymore. Biosimilars-lower-cost versions of complex biologic drugs used for cancer, arthritis, and autoimmune diseases-are now entering the market. As of 2023, 49 states and D.C. have laws covering biosimilar substitution. But the rules are all over the place.
Florida requires pharmacies to create a formulary that ensures substitutions won’t harm patients. Iowa tells pharmacists to rely on the FDA’s Orange Book. Hawaii still requires both doctor and patient consent for antiepileptic biosimilars. And in 2023, the FDA added 17 new therapeutic equivalence ratings just for biosimilars. That’s forced 23 states to review their laws.
There’s a push to fix this mess. The Uniform Law Commission drafted a Model State Biologics and Biosimilars Act in 2023 to bring some consistency. But until then, pharmacists are stuck juggling 49 different sets of rules.

How Pharmacists Keep Up
Managing this system isn’t easy. On average, a pharmacist spends 12.7 minutes per prescription checking state laws, FDA ratings, and patient history. That’s time they could spend talking to you about your meds. Most pharmacies now use software that auto-checks substitution rules based on your location and the drug. Eighty-three percent of pharmacy systems have this feature, and it cuts errors by 64%.
Pharmacy schools now teach 45 to 60 hours on state substitution laws. Nearly all states require it for licensing. But even then, mistakes happen. When a prescription crosses state lines-which happens in 18.3% of chain pharmacy transactions-it’s easy for a system to misread the rules. That’s why 78% of pharmacists say they’re confused when filling out-of-state prescriptions.
The Real Cost-And the Real Benefit
State laws aren’t just about money. They’re about access. In mandatory substitution states, generic fill rates average 94.1%. In permissive states, it’s 88.3%. That gap means thousands of patients aren’t getting the cheapest, most effective option.
But savings aren’t always the whole story. A 2022 survey found that 63% of pharmacists saw fewer patients abandon prescriptions when substitution was automatic. In Texas, abandonment for atorvastatin dropped by 15.2%. That’s huge. People who can’t afford their meds often skip doses or stop taking them entirely. Generic substitution helps keep them on track.
Still, there are trade-offs. The FDA’s MedWatch system recorded 217 patient complaints between 2020 and 2022 about side effects or lack of effectiveness after a switch. Most involved levothyroxine or warfarin. These aren’t random. They’re tied to NTI drugs. And while the FDA says generics are safe, real people report feeling different.
What’s Next?
The system is under pressure. The Congressional Budget Office estimates that if all 50 states aligned their laws, we could save an extra $8.7 billion by 2028. But patient advocates warn that pushing too hard for savings could hurt people with rare diseases or complex conditions. The National Organization for Rare Disorders says 25 to 30 million Americans rely on NTI drugs-and they need stability, not cost-cutting.
Right now, the U.S. has a system that saves billions but confuses patients and pharmacists alike. Some want one national standard. Others say states should keep control to protect local needs. Until that debate is settled, the pill you get tomorrow might depend on the zip code you live in.





Emma Sbarge
December 13, 2025 AT 13:27This patchwork of state laws is a national embarrassment. We’re talking about life-saving medication here, not which side of the road to drive on. If the FDA says it’s equivalent, then it’s equivalent. Why are we letting 50 different bureaucracies confuse patients and delay treatment? It’s time for a federal standard - no more state-by-state gambling with people’s health.
Pharmacists shouldn’t be legal scholars. They should be healthcare providers. This system is outdated, inefficient, and frankly, dangerous for people who can’t afford to miss a dose.
Stop hiding behind "local control." This isn’t about states’ rights - it’s about people dying because they can’t afford their meds and the system won’t let them get the cheaper version.
I’ve seen it firsthand. My mother skipped her levothyroxine for three months because she didn’t understand why the pill changed color. That’s not patient autonomy - that’s systemic failure.
Tommy Watson
December 14, 2025 AT 10:20so like… wait, you’re telling me i can’t just get the cheap pill if i want to? what the f***. why do i have to ask? i’m not a baby. just give me the generic and shut up. also why does my pill look different every time? i think they’re switching me to placebo on purpose lol.
also why is ny so extra? just say yes or no. i don’t wanna be interrogated at the pharmacy like i’m stealing something.
Donna Hammond
December 15, 2025 AT 18:08As a pharmacist with 14 years in community practice, I’ve seen the real impact of these laws - not just on costs, but on adherence. Patients on warfarin or levothyroxine who switch generics without proper counseling often panic. They think the drug isn’t working, or worse, that they’re being poisoned.
The solution isn’t banning substitution - it’s better communication. Every time a generic is dispensed, pharmacists should be required to give a 30-second verbal explanation: "This is the same medicine, just made by a different company. It’s FDA-approved and safe. If you feel different, call us."
Most patients just need to hear that. The software checks the law, but humans need reassurance. Training should include empathy, not just legal codes. And yes - we need federal alignment for NTI drugs. No state should be allowed to gamble with thyroid or seizure meds.
Also, biosimilars are the future. We’re already seeing 30% cost savings on rheumatoid arthritis drugs. But patients won’t trust them unless we explain it clearly. Stop treating patients like legal forms. Treat them like people.
Richard Ayres
December 16, 2025 AT 22:32This is a fascinating and deeply important issue that reveals how fragmented our healthcare system truly is. While the economic argument for generic substitution is overwhelming - $313 billion saved annually is staggering - the human dimension is often lost in policy debates.
The fact that 78% of pharmacists report confusion when filling out-of-state prescriptions suggests a systemic flaw in interoperability. It’s not just about laws - it’s about infrastructure. Pharmacy software needs to be standardized, and pharmacists need centralized, real-time legal updates - not 50 different PDFs from state boards.
Additionally, the emotional impact on patients deserves more attention. A pill’s color or shape triggers psychological associations. We assume patients understand bioequivalence, but many don’t. A simple sticker on the bottle - "This is a generic version. Same active ingredient. FDA-approved." - could reduce anxiety significantly.
Perhaps the answer isn’t uniformity in law, but uniformity in communication. We can preserve state autonomy while mandating patient education protocols. That’s a compromise that protects both access and trust.
Sheldon Bird
December 18, 2025 AT 10:00Man, this whole thing is wild but also kinda beautiful in a messed-up way. I’ve had my meds switched so many times I’ve started keeping a little notebook of what pills look like now vs. last month. I’m not mad - I’m just impressed the system works at all.
And honestly? I’m glad some states make you say yes. My cousin got switched to a generic for her seizure med and ended up in the ER. Not because it was unsafe - but because her body had adapted to that exact brand. It’s not about the science, it’s about the person.
Pharmacists are the real MVPs here. They’re juggling laws, software, and scared patients all day. We should be thanking them, not blaming them for the mess.
Also, I’m all for biosimilars. My dad’s arthritis med cost $1,200 a month. Now it’s $300. That’s life-changing. Let’s keep pushing that forward - just make sure we don’t lose the human touch along the way. ❤️
Karen Mccullouch
December 19, 2025 AT 04:36THIS IS WHY AMERICA IS FALLING APART. You think it’s about money? No. It’s about control. Big Pharma doesn’t want generics. States are just doing their bidding. And now we’ve got pharmacists playing lawyer because some bureaucrat in Kentucky thinks levothyroxine is a weapon of mass destruction.
My sister got switched to a generic for her thyroid and her heart started racing. She went to the ER. The doctor said, "It’s the same chemical." But she felt different. And guess what? Her body knows better than some FDA database.
Stop forcing people to take cheap pills. If you want to save money, tax the rich. Don’t make sick people gamble with their health because some politician thinks generics are "patriotic."
And don’t even get me started on biosimilars. Those are just brand-name drugs with a new label and a 70% discount. You think the companies don’t know this? They’re laughing all the way to the bank.
Michael Gardner
December 19, 2025 AT 21:29Wait - you said 92.5% of prescriptions are for generics? Then why are we even talking about this? If the system works so well, why are we making it more complicated? Maybe the problem isn’t the laws - maybe it’s that people are overthinking it.
Also, I’ve taken generics for 15 years. I’ve never felt a difference. So why are we treating patients like they’re fragile glass figurines? Maybe the real issue is that people don’t trust medicine anymore - not because of generics, but because of corporate greed and bad PR.
And if biosimilars are so different, why does the FDA approve them? If they’re not equivalent, they shouldn’t be allowed. If they are, then stop making it a mystery.
Willie Onst
December 21, 2025 AT 16:42It’s funny - this whole thing reminds me of how different states have different rules for who can sell beer on Sunday. We’ve been doing this kind of patchwork for centuries. But with medicine, it’s not about tradition - it’s about survival.
I’ve lived in six states. I’ve had my blood thinner switched, my thyroid med switched, even my antidepressant switched. Some places asked me. Some didn’t. One pharmacist in Ohio just handed me the new pill and said, "You good?" I said yes. He nodded. That’s it.
Maybe we don’t need more laws. Maybe we need more trust. Trust in pharmacists. Trust in science. Trust that people can make their own choices - if they’re given the facts.
And hey - if you’re worried about your meds, ask. Just say, "Can you tell me what changed?" Most pharmacists will sit down with you for ten minutes. They want you to be safe. They’re not the enemy. The system is.