When you’re juggling multiple prescriptions, supplements, or even a favorite snack, a quick check for harmful combos can feel like a lifesaver. Two names keep popping up in Google results - the FDA and WebMD - each offering a way to spot risky interactions. But they work very differently, and using them the wrong way can give you a false sense of security.
What the FDA Actually Offers
FDA Drug Interaction Checker is not a public‑facing tool at all. The U.S. Food and Drug Administration, created by the 1906 Pure Food and Drug Act and formally named in 1930, monitors drug safety through post‑market surveillance, adverse event reporting, and recalls. While the agency maintains the FDA Adverse Event Reporting System (FAERS) and publishes safety communications, it does not host a searchable interaction database for consumers. Instead, it relies on manufacturers to submit interaction data, which the FDA then reviews and incorporates into labeling.
Why does this matter? Because the FDA’s strength lies in official, legally binding safety information, but the lack of a simple, free checker means patients often turn to third‑party sites for quick answers.
WebMD’s Consumer‑Friendly Checker
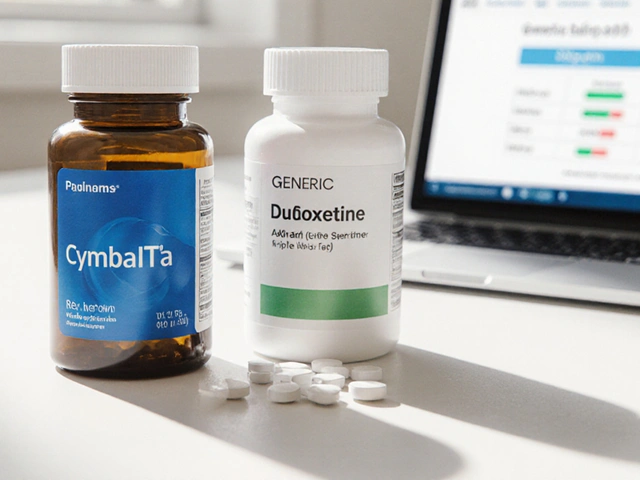
WebMD Drug Interaction Checker is a free, web‑based tool launched in the early 2000s. It lets anyone type in an unlimited list of drugs, supplements, or foods and get a rapid read‑out of possible drug‑drug, drug‑food, and drug‑condition interactions. The content is medically reviewed by pharmacists like Joshua Conrad, PharmD, and the platform updates its database regularly (last major update September 15 2023).
Key features:
- No registration required - just a browser and an internet connection.
- Results appear in under three seconds for typical queries.
- Visual severity icons (minor, moderate, major) aimed at a lay audience.
What it doesn’t do:
- It lacks detailed pharmacokinetic explanations (e.g., cytochrome P450 pathways).
- Herbal and supplement coverage is still incomplete despite a 2023 update adding 1,200 new herbal compounds.
- It provides no API for EHR integration, so clinicians can’t embed it directly into their workflow.
Side‑by‑Side Comparison (FDA vs. WebMD vs. DrugBank)
| Feature | FDA (official) | WebMD (consumer) | DrugBank (commercial) |
|---|---|---|---|
| Public access | No standalone checker | Free, unlimited queries | Free tier: up to 5 drugs; paid API for unlimited |
| Depth of pharmacology | Label‑based, regulatory summaries | Basic interaction lists, no enzyme info | Cytochrome P450 pathways, pharmacogenomics (enterprise) |
| Update frequency | Aligned with FDA safety communications (as needed) | Quarterly major updates; supplement add‑on 2023 | Real‑time FDA adverse event feed (Dec 2023) |
| Integration options | None for consumers | Web UI only | FHIR‑compatible API, 99.9% uptime SLA |
| Cost | Free (government) | Ad‑supported, no direct fees | $1,200/mo for 10,000 queries (enterprise) |
| Known limitations | No consumer tool; relies on manufacturers’ data | May miss herb‑drug combos; occasional outdated alerts | Free tier omits pharmacogenomics; steep pricing for small practices |
Best Practices for Safe Use
Even the best checker can’t replace a pharmacist or physician. Treat any result as a *starting point*, not a final verdict. Follow these steps each time you run a query:
- List every substance you’re taking. Include prescription meds, over‑the‑counter pain relievers, vitamins, herbs, and even common foods (e.g., grapefruit, cranberry juice).
- Enter the full, generic name. Brand names can map to multiple ingredients and cause mismatches.
- Read both the interaction description and the severity icon. Remember that “moderate” still accounts for roughly 18% of preventable hospital admissions (Ann Intern Med 2021).
- Cross‑check high‑risk combos (e.g., warfarin + leafy greens, NSAIDs + heart failure) with a second source such as the FDA safety communication archive or a professional database like DrugBank.
- If the checker flags an interaction, note the mechanism (enzyme inhibition, additive side‑effects) and bring it to your clinician’s attention.
- Document the date of the query. Interaction databases can lag by 12-18 months for new drugs, so a later check may reveal a previously hidden risk.
Integrating Checkers Into Personal Health Management
For patients who self‑manage chronic conditions, a simple workflow can keep safety top‑of‑mind:
- Morning scan. Before breakfast, pull up the WebMD checker on your phone and type in today's meds plus any new supplement you plan to take.
- Weekly review. Every Sunday, run a broader search that includes all meds you’ve been prescribed in the last month. Save the PDF snapshot in a cloud folder labeled “Medication Safety”.
- Clinician share. Upload the snapshot to your patient portal or email it to your pharmacy before the next appointment. Most EHRs allow you to attach PDFs directly to the visit note.
For clinicians, the workflow flips: use the FDA’s labeling information and DrugBank’s API during chart review, then confirm any questionable alerts with a patient‑friendly tool like WebMD to explain the risk in plain language.
Common Pitfalls and How to Avoid Them
Even experienced users stumble. Here are the top three traps and quick fixes:
| Pitfall | Why It Happens | Remedy |
|---|---|---|
| Relying on severity icons alone | Icons are simplified for laypeople and may hide clinical nuance. | Read the full text description; ask your pharmacist about the mechanism. |
| Skipping supplement entries | Many tools treat vitamins as “non‑drugs”. | Always add supplements and foods manually, even if you think they’re harmless. |
| Assuming the database is up‑to‑date | New drugs (e.g., fedratinib) can be missing for months. | Check the FDA’s latest safety communication for any newly approved agents. |
When to Call a Professional
If any of the following occur, stop the DIY routine and pick up the phone:
- You see a “major” interaction involving a medication with a narrow therapeutic index (e.g., warfarin, digoxin, lithium).
- You have a chronic condition that changes drug metabolism, such as renal impairment in 28% of elderly patients (JAMA Int Med 2021).
- The checker returns “no interactions” but you’re experiencing new side effects - could be a rare interaction not yet cataloged.
Remember, both the FDA and WebMD explicitly state that their tools do not replace professional medical advice.

Future Directions - AI, Real‑Time Feeds, and Explainability
The landscape is shifting fast. By 2026, the FDA’s Digital Health Innovation Action Plan will require all certified interaction checkers to provide explainable AI trails - essentially a “why” for each prediction. Google’s Med‑PaLM 2 already hits 89% accuracy in predicting novel interactions, but LLM hallucinations still affect 22% of outputs. Expect newer versions of WebMD and DrugBank to embed AI explanations, linking each alert to primary literature, clinical trial data, or FDA adverse event reports.
Real‑time feeds, like DrugBank’s December 2023 integration of the FDA’s adverse event stream, mean that today’s checker can flag a newly reported interaction within hours instead of weeks. For patients, that translates to quicker warnings about emerging risks (e.g., a new antiplatelet causing bleeding when mixed with a novel anticoagulant).
Quick Recap Checklist
- Identify every medication, supplement, and food you take.
- Use WebMD for a fast, consumer‑level scan.
- Cross‑verify high‑risk alerts with FDA safety communications or DrugBank’s API.
- Document the date and version of the checker used.
- Never replace a pharmacist’s review with a web tool.
Frequently Asked Questions
Does the FDA provide a free drug interaction checker for patients?
No. The FDA monitors drug safety through labeling, adverse event reporting, and recalls, but it does not host a public‑facing interaction checker. Clinicians can access FDA safety communications, and manufacturers must submit interaction data to the agency.
How reliable is WebMD’s interaction checker?
WebMD catches about 85% of high‑risk interactions, according to its own review. It excels at user‑friendly explanations but can miss newer drug‑herb combos and sometimes lags behind FDA updates by several months.
When should I trust a “moderate” interaction warning?
Treat moderate alerts seriously. Studies show they account for roughly 18% of preventable hospital admissions. Always discuss them with a pharmacist or doctor, especially if you have kidney issues or are on a medication with a narrow therapeutic window.
Can I use WebMD’s checker on my phone without an internet connection?
No. The tool runs entirely in the browser and needs an active internet connection to retrieve the latest database.
Is there a free version of DrugBank that I can use at home?
DrugBank offers a limited free tier that lets you check up to five drugs at a time. For deeper pharmacokinetic details or API access, a paid subscription is required.
By treating these tools as part of a broader safety net-always backed by a health professional-you’ll reduce the odds of a nasty, avoidable interaction.






sarah basarya
October 26, 2025 AT 17:12If you think WebMD is a magic bullet, you’re living in a fantasy.
Ben Dover
October 28, 2025 AT 10:52While the author extols the virtues of WebMD’s consumer-friendly interface, the underlying epistemic scaffolding remains woefully simplistic. The FDA, by contrast, operates within a regulatory paradigm that demands rigorous post‑marketing surveillance and statutory compliance. It is imperative to recognize that the absence of a public‑facing interaction checker is a deliberate manifestation of statutory constraints rather than an oversight. Moreover, the reliance on manufacturer‑submitted data introduces a latency that can obscure nascent adverse event signals. WebMD’s database, although updated quarterly, frequently lags behind the FDA’s adverse event feed by several months, thereby compromising temporal fidelity. Users must therefore treat WebMD’s severity icons as heuristic approximations, not deterministic verdicts. A prudent strategy involves cross‑referencing any flagged interaction with the FDA’s safety communications or an evidence‑based repository such as DrugBank. Ultimately, the onus lies with the patient to synthesize multiple data streams rather than capitulate to a single, user‑centric portal.
Ben Durham
October 30, 2025 AT 04:32Let’s break down the workflow step by step so it feels less overwhelming. First, write down every prescription, over‑the‑counter product, vitamin, herb, and even food items you consume on a daily basis. Next, enter the generic names into the WebMD checker to obtain an initial interaction profile; the tool will highlight minor, moderate, and major alerts with distinct icons. After you obtain the results, consult the FDA’s safety communication archive for any high‑risk alerts that may not appear in the consumer database. If a moderate or major interaction surfaces, note the mechanistic rationale-whether it’s enzyme inhibition or additive toxicity-and bring this note to your pharmacist or physician. Finally, archive the PDF snapshot in a cloud folder labeled “Medication Safety” and share it via your patient portal before your next appointment. By iterating this routine weekly, you create a safety net that supplements professional oversight.
Tony Stolfa
October 31, 2025 AT 22:12Jesus, you sound like you’ve never actually clicked a button on WebMD. Stop over‑analyzing the user experience and just admit the tool works fine for most people. Yes, the data isn’t perfect, but it’s better than flying blind in your own kitchen. If you want a perfect system, go build one yourself instead of whining about constraints. Bottom line: use it, double‑check with your doc, and quit the academic drivel.
Leah Ackerson
November 2, 2025 AT 15:52We all chase the illusion of absolute safety, yet the universe thrives on uncertainty 🌌. Embracing a tool like WebMD is akin to holding a candle in a storm; it offers illumination but never guarantees shelter. The real wisdom lies in recognizing that each interaction flag is a philosophical prompt to question how our bodies negotiate chemistry. When a “moderate” warning flashes, ponder the delicate balance between benefit and risk, rather than merely fearing the label. In the grand tapestry of health, we are both the weaver and the thread, constantly adjusting our patterns. So, let the icons guide you, but let your curiosity steer the conversation with your caregiver. 🌱💡
renee granados
November 4, 2025 AT 09:32Don’t trust those big pharma sites – they hide the real risks. They want you to think a pop‑up warning is enough, but the truth is buried.
Stephen Lenzovich
November 6, 2025 AT 03:12The notion that a free, ad‑supported checker can supplant a clinician’s expertise is a narrative woven by profit‑driven platforms seeking user engagement at the expense of nuanced care. First, the FDA’s regulatory framework is deliberately opaque to the lay public because it safeguards against misinterpretation of complex pharmacovigilance data, a reality many ignore. Second, WebMD’s user interface, while slick, simplifies intricate pharmacokinetic pathways into smiley faces, which can lull users into a false sense of mastery over their medication regimens. Moreover, the frequent lag in updating herb‑drug interactions creates a temporal blind spot precisely when new supplements flood the market, a gap that has manifested in several documented cases of unexpected bleeding events. Third, the algorithmic prioritization of “major” versus “moderate” alerts lacks context about comorbidities, renal function, or genetic polymorphisms that could dramatically alter risk stratification. Fourth, the reliance on manufacturer‑submitted data means that any conflict of interest inherent in the pharmaceutical supply chain propagates into the very alerts presented to patients. Fifth, the absence of integration with electronic health records precludes real‑time cross‑validation, forcing the onus entirely onto patients who may not have the requisite health literacy. Sixth, the cultural bias embedded in most Western drug interaction databases often overlooks ethnopharmacological nuances relevant to minority populations, further eroding equity. Seventh, the simple act of entering a drug name can produce mismatches due to brand versus generic variations, leading to either missed interactions or spurious warnings that erode trust. Eighth, the psychological impact of receiving a “major” alert without professional mediation can induce anxiety, potentially prompting patients to discontinue essential therapy without guidance. Ninth, the commercial model underpinning WebMD-advertising revenue tied to page views-creates an incentive structure where frequent alerts may increase traffic, a subtle form of monetization that skirts ethical lines. Tenth, as AI begins to anticipate novel interactions, the current static databases risk becoming obsolete unless they adapt swiftly, a transition that many legacy platforms have struggled to achieve. Eleventh, the cumulative effect of these shortcomings is a systemic vulnerability that can culminate in preventable adverse drug events, the very outcome these tools promise to avert. Finally, the prudent approach combines the convenience of a consumer‑friendly checker with the rigor of professional oversight, ensuring that technology serves as a supplement rather than a substitute for clinical judgment. In essence, technology is a tool, not a tyrant, and we must wield it wisely.
abidemi adekitan
November 7, 2025 AT 20:52Hey there, fellow health‑navigator! 🌈 You’ve painted a vivid picture of the pitfalls, and that’s exactly why we need to treat these tools as a collaborative canvas rather than a lone masterpiece. Think of the WebMD checker as a bright splash of color-quick, eye‑catching, and useful for spotting glaring contrast. Then, bring in the FDA’s regulatory brushstrokes and the deep‑textured layers of DrugBank for those nuanced details that give the painting its depth. By layering these resources, you create a richer, more resilient portrait of medication safety. Keep experimenting, share your drafts with your care team, and remember: the best art is always a dialogue, not a solo act.
Barbara Ventura
November 9, 2025 AT 14:32Wow, this thread is a treasure‑trove of insights, and I can’t help but notice how each perspective adds a new dimension, from regulatory nuance to user‑experience simplicity, from AI‑driven forecasts to good‑old pharmacist wisdom, and even a dash of philosophical reflection, all of which converge to remind us that medication safety is a collective responsibility, not a solitary endeavor.
laura balfour
November 11, 2025 AT 08:12Honestly, reading through all these comments feels like watching a blockbuster movie where the heroes-WebMD, the FDA, and our very own healthcare providers-team up against the villainous shadows of drug interactions. It’s a bit like the plot twists in a soap that keep you on the edge of your seat, only the stakes are our health. Sure, some of the info can be a lil confusing-y’know, that “herb‑drug” thingy-but when we all chip in, we get a clearer picture. So let’s keep the dialogue rolling, keep the drama alive, and make sure no one gets left behind in the credits.