Melanoma is the deadliest form of skin cancer, but it’s also one of the most preventable-if you know what to look for and act fast. Every year in the U.S., over 100,000 new invasive cases are diagnosed. The good news? If caught early, the five-year survival rate is over 99%. The bad news? If it spreads, that number drops to 35%. This isn’t just a summer problem. It’s a year-round risk, and it doesn’t care if you have light skin or dark skin. What matters is how you protect yourself, how often you check your skin, and what you do when something looks off.
What Melanoma Really Is
Melanoma starts in melanocytes-the cells that give your skin its color. These cells can turn cancerous after too much UV exposure from the sun or tanning beds. Unlike other skin cancers that grow slowly, melanoma can spread quickly to lymph nodes and organs like the lungs or brain. That’s why it kills more people than basal cell or squamous cell carcinomas, even though it makes up less than 1% of all skin cancers.
There are four main types:
- Superficial spreading melanoma (70% of cases)-the most common. It spreads sideways across the skin before digging deeper.
- Nodular melanoma (15-30%)-grows fast and looks like a raised bump. Often black or dark, but can be pink or red.
- Lentigo maligna melanoma (10-15%)-shows up on sun-damaged skin, usually on the face or arms of older adults.
- Acral lentiginous melanoma (2-8%)-appears on palms, soles, or under nails. More common in people with darker skin tones, and often missed because it doesn’t look like typical sun damage.
That last type is critical to understand. Many Black and brown patients are diagnosed late because doctors and even patients assume melanoma only happens on sun-exposed skin. But it can hide under a nail, on the foot, or on the scalp. That’s why self-checks matter for everyone.
How to Prevent Melanoma
Up to 90% of melanomas are caused by UV radiation. That means most cases are preventable. But prevention isn’t just about sunscreen.
Here’s what actually works:
- Use broad-spectrum SPF 30+ daily-even on cloudy days. UVA rays penetrate clouds and windows. Reapply every two hours, or after sweating or swimming.
- Avoid tanning beds completely. Using them before age 35 increases melanoma risk by 75%. That’s not a myth-it’s backed by data from the British Journal of Dermatology.
- Seek shade between 10 a.m. and 4 p.m. That’s when UV rays are strongest. Wear wide-brimmed hats, UV-blocking sunglasses, and tightly woven clothing.
- Check the UV index. Apps like QSun or the EPA’s SunWise tool give real-time UV levels. When it’s 6 or higher, take extra precautions.
- Protect kids. Childhood sunburns double melanoma risk later in life. Don’t wait until they’re teens to teach sun safety.
Here’s a hard truth: Only 14% of U.S. high schoolers use sunscreen regularly. Cost is a barrier for many families. But a $10 bottle of sunscreen lasts months. Spending $30 a year on protection saves thousands in treatment costs. The CDC says every $1 spent on UV prevention saves $3.50 in medical bills.
How to Detect Melanoma Early
Early detection saves lives. The ABCDE rule is your first tool:
- Asymmetry-One half doesn’t match the other.
- Border irregularity-Edges are ragged, notched, or blurred.
- Color variation-Shades of brown, black, red, white, or blue within the same spot.
- Diameter-Larger than 6mm (about the size of a pencil eraser). But melanomas can be smaller.
- Evolving-Changing in size, shape, color, or texture over weeks or months.
Don’t wait for all five signs. If a mole is changing, it’s enough to get it checked. Also watch for:
- A spot that bleeds, itches, or crusts without healing.
- A new dark streak under a nail.
- A sore that won’t go away.
- A mole that looks different from all the others (the “ugly duckling” sign).
Do a self-exam once a month. Take 10-15 minutes after a shower. Use a mirror to check hard-to-see areas: back, scalp, between toes, under breasts. Take photos with your phone to track changes over time.
Teledermatology is now an option for many. A 2023 study found it’s 87% accurate compared to in-person visits. But it’s not perfect. If something feels wrong, don’t rely on a photo alone. Go in person.
What Happens When Melanoma Is Found
If your doctor sees something suspicious, they’ll do a biopsy. That’s when a small piece of skin is removed and checked under a microscope. No guesswork. No waiting. Just facts.
Staging tells you how far it’s gone:
- Stage 0 (in situ)-Cancer is only in the top layer of skin. Surgery removes it. Cure rate: nearly 100%.
- Stage I-II-Tumor is deeper but hasn’t spread. Surgery with wider margins (1-2 cm) is standard. A sentinel lymph node biopsy may be done if the tumor is over 0.8mm thick.
- Stage III-Cancer reached nearby lymph nodes. Surgery plus immunotherapy (like nivolumab or pembrolizumab) is now standard. These drugs help your immune system fight the cancer.
- Stage IV-Spread to distant organs. Treatment is more complex. Immunotherapy or targeted therapy (for BRAF-mutant tumors) can extend life for years.
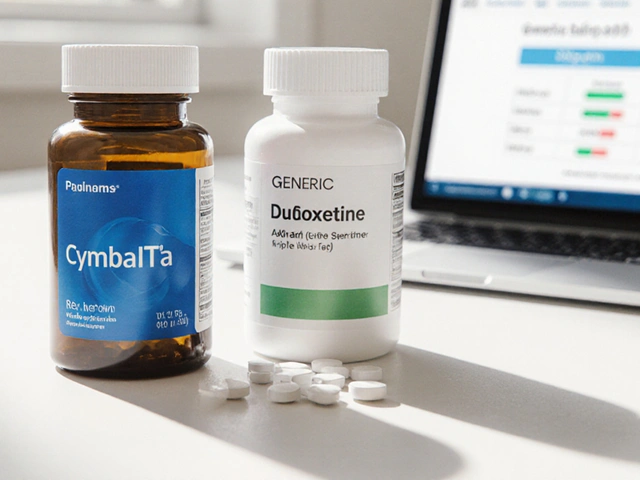
Genetic testing is now routine for Stage IIB and above. About half of melanomas have a BRAF mutation. If yours does, drugs like dabrafenib and trametinib can be very effective. But they come with side effects-rash, fever, fatigue-and cost up to $200,000 a year.
Immunotherapy works better long-term. In the CheckMate 067 trial, 52% of Stage IV patients were still alive after five years. But it takes months to kick in. Targeted therapy works faster-sometimes in weeks-but doesn’t last as long.
Real Stories, Real Risks
One woman in Manchester, 42, noticed a dark spot under her big toe. She thought it was a bruise from her shoes. Six months later, it was Stage III acral melanoma. She had a toe amputation and now gets immunotherapy every three weeks. “I didn’t know melanoma could hide there,” she told me.
A 19-year-old student used a UV index app and noticed his freckle had grown. He got it checked. It was a 0.4mm melanoma. Removed in 20 minutes. No chemo. No hospital stay. Just a quick excision. His survival odds? 99.6%.
But not everyone is so lucky. On Reddit, a man posted about paying $28,500 out of pocket for one infusion of nivolumab-even with insurance. That’s not rare. Treatment costs for melanoma hit $3.4 billion in the U.S. last year. And many rural areas have no dermatologists within 50 miles.
People of color face another barrier: misdiagnosis. A 2024 study found Black patients were twice as likely to be told a melanoma was a “bruise” or “infection.” That’s why knowing your own skin matters more than ever.
What’s New in 2025
The field is moving fast. In early 2025, the FDA approved two major advances:
- DermEngine’s VisualizeAI-an AI tool that analyzes skin images and flags high-risk lesions with 93.2% accuracy. It’s being rolled out in clinics across the U.S.
- mRNA-4157/V940-a personalized vaccine made from your own tumor’s DNA. When combined with pembrolizumab, it cut recurrence risk by 44% in high-risk patients.
Also, the CDC is now pushing UV index alerts into weather apps. By 2026, 120 million people will get daily UV warnings on their phones. And Walmart is testing teledermatology kiosks in 150 clinics-aimed at rural communities with no dermatologists.
But progress won’t reach everyone unless we fix access. The richest Americans are seeing declining melanoma rates. The poorest? Rates are still rising. Prevention isn’t just about science. It’s about equity.
What You Should Do Right Now
You don’t need to wait for a doctor’s appointment to protect yourself. Here’s your action plan:
- Check your skin this week. Use the ABCDE rule. Take a photo of anything new or changing.
- Apply sunscreen daily. Don’t skip it because it’s cloudy or you’re indoors.
- Stop using tanning beds. There’s no safe tan.
- Know your risk. Fair skin? More than 50 moles? Family history? Get a professional exam every 6 months.
- Ask for help. If you can’t afford sunscreen, ask at your local clinic. Many offer free samples. If you can’t get a dermatologist appointment, try teledermatology.
Melanoma isn’t inevitable. It’s not fate. It’s a result of exposure, delay, and sometimes, neglect. But with the right knowledge and action, you can stop it before it starts-or catch it when it’s still curable.
Can melanoma be cured if caught early?
Yes. When melanoma is found in its earliest stage-before it goes deeper than 1mm-the five-year survival rate is over 99%. Surgery alone is often enough to remove it completely. Early detection is the single most effective way to survive melanoma.
Is melanoma only a risk for fair-skinned people?
No. While fair-skinned people have a higher risk, melanoma is often diagnosed later in people with darker skin. It commonly appears on palms, soles, under nails, or in the mouth. These are the hardest spots to notice, and they’re often mistaken for bruises or infections. Everyone, regardless of skin tone, needs to check their skin regularly.
Do I need to get a skin check every year?
If you’re at average risk, a yearly exam is fine. But if you have more than 50 moles, a family history of melanoma, or a history of sunburns, you should go every 3 to 6 months. High-risk people also benefit from total body photography, which tracks changes over time.
Can sunscreen prevent melanoma completely?
Sunscreen reduces your risk significantly, but it doesn’t eliminate it. You also need to avoid peak sun hours, wear protective clothing, and avoid tanning beds. Think of sunscreen as one layer of protection-not the whole shield.
Are new melanoma treatments too expensive?
Yes, some are. Immunotherapy and targeted drugs can cost over $150,000 a year. But many patients qualify for financial aid through drug manufacturers, nonprofits like the Melanoma Research Foundation, or Medicaid expansion. Always ask your oncology team about assistance programs. You’re not alone in this cost.
Can I rely on smartphone apps to detect melanoma?
Apps can help you track changes, but they’re not diagnostic tools. AI tools like DermEngine are used by doctors, not consumers. If an app flags something, still see a dermatologist. Never skip a professional evaluation for an app result.





Julie Roe
November 18, 2025 AT 00:01I’ve been doing monthly skin checks since my cousin got diagnosed with melanoma at 28. Took me a while to get into the habit, but now I take pics of my moles every first of the month. One time I caught a weird dark line under my pinky nail-turned out it was just a bruise, but I’m glad I checked. Honestly, if I hadn’t been looking, I might’ve ignored it until it was too late. Everyone deserves to know their own body, no matter your skin tone or how busy you are. Just 10 minutes a month could save your life.
jalyssa chea
November 18, 2025 AT 05:10why do people think sunscreen is enough i mean seriously its not a force field you still get burned through clouds and windows and dont even get me started on tanning beds i used to use them cause i thought it looked good now i regret it so much like why do we do this to ourselves
Gary Lam
November 18, 2025 AT 08:55So let me get this straight-our government is pushing UV alerts into weather apps, Walmart’s putting telederm kiosks in stores, and AI can spot melanoma better than some docs… but people still think it’s just a ‘summer thing’? 😂 We’re living in the future and some folks are still using 1998 logic. Also, if you’re not checking under your nails, you’re basically playing Russian roulette with your skin. Not cool.
Peter Stephen .O
November 19, 2025 AT 10:28Bro this post hit different. I used to think melanoma was just for pale people who sunbathed like it was a job. Then my uncle got diagnosed with a black streak under his toenail-he thought it was dirt. Turns out it was acral melanoma. He lost his toe. But he’s alive because he finally went to the doc. I started using sunscreen daily even when I’m indoors. I even got my mom to download a skin tracker app. It’s not just about looking good-it’s about staying alive. And yeah, the cost of treatment is insane, but the price of ignoring it? Way higher. Don’t wait for a warning sign. Be the person who checks their own skin before it’s too late.
Andrew Cairney
November 20, 2025 AT 14:06AI skin scanners? mRNA vaccines? Telederm kiosks? This is all a distraction. The real cause? 5G radiation + chemtrails + glyphosate in sunscreen. They’re testing melanoma on us to justify selling $200k drugs. Look at the stats-rates are rising in rural areas? That’s because they’re not giving out the ‘real’ sunscreen. The CDC’s UV alerts? Just a way to get you to buy more products. I checked my mole. It’s fine. I’m not falling for the scam. 🤡
Rob Goldstein
November 21, 2025 AT 04:35Just wanted to clarify something about staging and treatment protocols. For Stage IIB and above, BRAF testing is now standard of care-not optional. If you’re BRAF-positive, combo therapy with dabrafenib + trametinib has shown median progression-free survival of over 11 months in clinical trials. Immunotherapy with anti-PD1 agents like pembrolizumab has better durability but slower onset. The key is early biopsy and molecular profiling. Don’t delay referral to a melanoma specialist. And yes, financial toxicity is real-many pharma companies offer co-pay assistance programs. Reach out to the Melanoma Research Foundation-they’ve helped thousands. You’re not alone in this.
vinod mali
November 21, 2025 AT 19:24My cousin in India got melanoma on his palm. No one believed him. Said it was dirt from work. Took 8 months to get a biopsy. Now he’s on immunotherapy. I told my family to check their hands and feet. We don’t have dermatologists nearby but we take photos and send them to a doctor online. It’s not perfect but better than waiting. Sunscreen is expensive here but we use hats and shade. Small things matter. Everyone should look at their skin. Not just the face.
Jennie Zhu
November 23, 2025 AT 12:02It is imperative to underscore the clinical significance of the ABCDE criteria as a foundational diagnostic heuristic in dermatological oncology. Furthermore, the integration of teledermatology platforms, while promising, must be contextualized within the framework of evidence-based triage protocols. The financial burden of targeted therapies remains a critical public health concern, necessitating policy intervention to ensure equitable access to life-saving interventions. Early detection remains the cornerstone of improved survival outcomes, and adherence to monthly self-examinations should be institutionalized within primary care frameworks.
Kathy Grant
November 25, 2025 AT 03:55I used to think skin cancer was something that happened to other people. Then I saw my best friend cry because she had to tell her 10-year-old daughter she might lose her leg. She didn’t notice the spot under her foot until it was bleeding. That’s the thing about melanoma-it doesn’t scream. It whispers. And if you’re not listening, if you’re too busy, too scared, too used to ignoring your body… it just keeps growing. I started checking my skin every week. Took pictures. Talked to my kids about it. I don’t want to be the person who says ‘I didn’t know.’ I know now. And I won’t look away again.