AB Code: What It Means and How It Affects Your Medications
When you pick up a generic prescription, you might see an AB code, a rating assigned by the FDA to indicate therapeutic equivalence between a brand-name drug and its generic version. Also known as therapeutic equivalence code, it's not just a label—it's your assurance that the generic you're taking will work the same way as the brand, with the same active ingredients, strength, and absorption rate. Not all generics carry an AB code. Some are rated BX, meaning they’re not considered interchangeable, often because their absorption varies too much between batches or they’re complex formulations like extended-release pills.
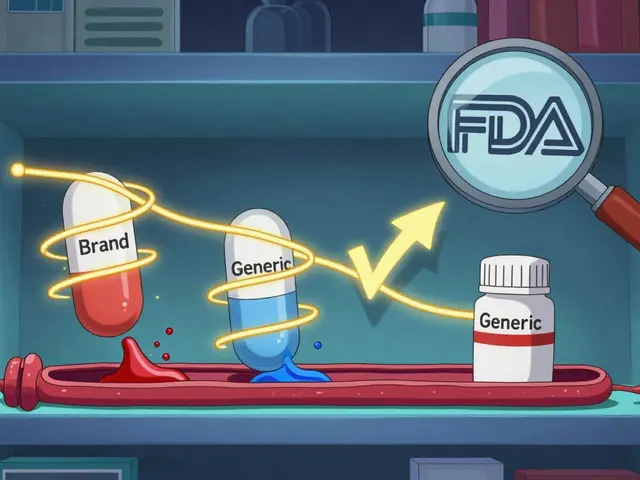
The FDA, the U.S. agency responsible for evaluating drug safety and effectiveness uses strict testing to assign these codes. For a drug to get an AB rating, it must pass bioequivalence studies—proving it releases the same amount of medicine into your bloodstream at the same speed as the brand. This matters because even small differences in absorption can affect how well a drug works, especially for medications like seizure drugs, blood thinners, or thyroid pills where precision is critical.
Generic drugs, lower-cost versions of brand-name medications that contain the same active ingredient are everywhere now, and most are safe and effective. But if your doctor or pharmacist switches your prescription without checking the AB code, you could end up with a version that doesn’t work the same way. That’s why it’s important to know what’s in your pill bottle. Some pharmacies automatically substitute generics, even when the prescriber didn’t intend it. And while most AB-rated generics perform just like the brand, others—especially those without the code—might cause side effects or treatment failure.
This is why so many of the articles here focus on generic medication safety, drug interactions, and how to spot the difference between true equivalents and questionable substitutes. You’ll find guides on how to read your prescription label for the AB code, what to do if your generic suddenly stops working, and why some doctors avoid switching to generics altogether. You’ll also learn how storage, expiration dates, and even the filler ingredients in generics can affect how your body responds.
Whether you’re on a tight budget, switching insurers, or just trying to understand why your medication feels different, knowing about AB codes gives you real control. You don’t have to guess whether your generic is safe. You can ask. You can check. You can demand the right version. Below, you’ll find real-world advice from people who’ve been there—how to spot red flags, how to talk to your pharmacist, and when to insist on staying with the brand. This isn’t about fear. It’s about knowing exactly what you’re taking—and why it matters.

Therapeutic Equivalence Codes: How the FDA Determines Which Generic Drugs Can Be Substituted
The FDA uses therapeutic equivalence codes to determine which generic drugs can be safely substituted for brand-name medications. Learn how the A and B codes work, why some generics aren't interchangeable, and how this system saves billions in healthcare costs.