After a broken wrist, a sprained ankle, or even minor surgery, most people expect pain to fade over weeks. But for some, the pain doesn’t just stick around-it gets worse. It starts as a dull ache, then turns into a constant burning sensation, like your skin is on fire. A light touch, a breeze, or even a change in room temperature can feel unbearable. This isn’t normal healing. This is Complex Regional Pain Syndrome, or CRPS.
What Exactly Is CRPS?
CRPS is a neurological disorder that causes severe, long-lasting pain after an injury. It’s not just pain from damaged tissue-it’s pain from your nervous system going haywire. Your brain keeps receiving pain signals even when the injury has healed. This isn’t in your head. It’s a real, measurable dysfunction in how nerves communicate with your brain.
There are two types. Type I, which makes up about 90% of cases, happens after an injury with no clear nerve damage-like a fracture or sprain. Type II follows a confirmed nerve injury, such as from a cut or surgical complication. Both types cause the same symptoms: intense burning, throbbing, or stabbing pain that’s way out of proportion to what you’d expect.
CRPS usually affects arms or legs, but it can happen anywhere. It’s not rare-it’s just often missed. Around 20 to 50 people per 100,000 develop it each year in the UK. Women are three times more likely to get it than men, and it’s most common between ages 40 and 60. But younger people can get it too.
Why Does It Feel Like Fire?
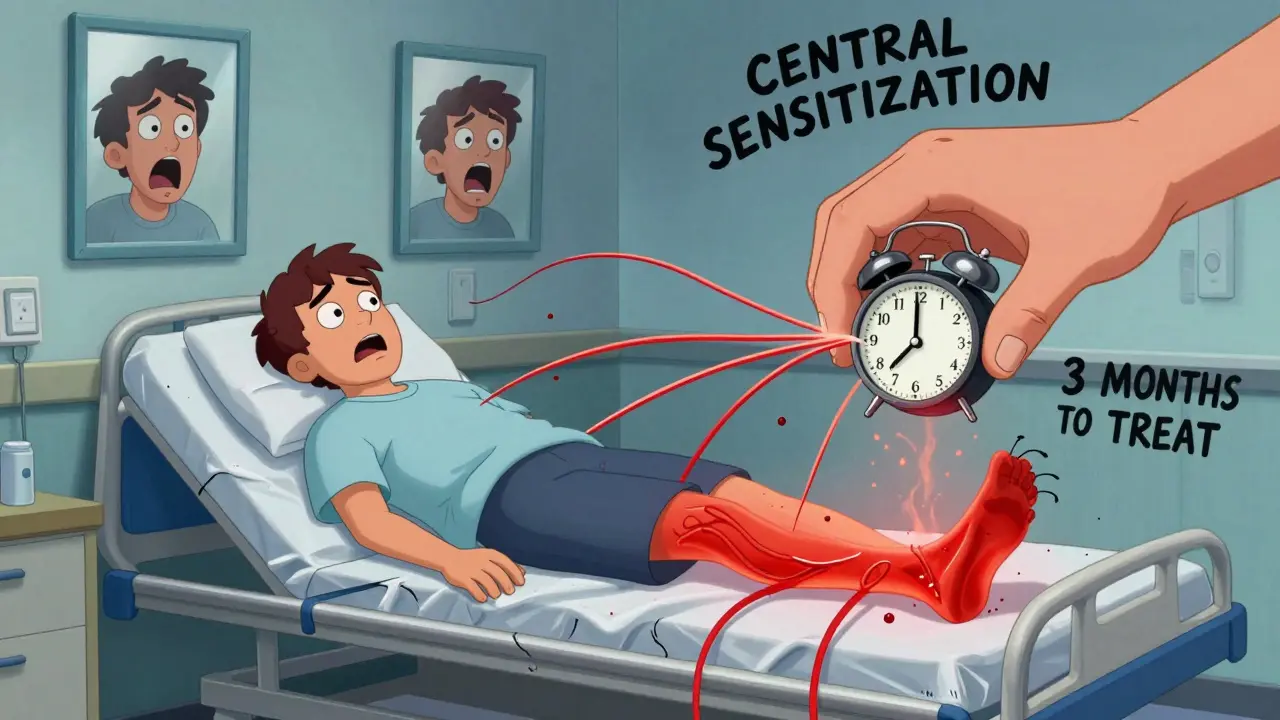
The burning pain isn’t just a description-it’s what’s happening in your nerves. Tiny nerve fibers, called C-fibers, become overactive and send constant pain signals. Your spinal cord and brain start interpreting even harmless sensations as dangerous. This is called central sensitization. It’s like your nervous system’s alarm system got stuck on high volume.
Early on, the affected limb might feel warmer than the other side. Later, it can turn cold, pale, or blotchy. Skin becomes thin, shiny, and overly sensitive. You might notice hair or nails growing faster or slower than usual. Swelling, stiffness, and muscle spasms are common. Some people lose the ability to move their fingers or toes properly. The pain doesn’t just hurt-it makes everyday life impossible.
One key sign? Temperature differences between limbs. Studies show the affected limb can be 0.5°C to 1.5°C warmer or cooler than the healthy one. That’s enough for trained doctors to spot during an exam. If you’ve had an injury and your skin feels strangely hot or cold compared to the other side, that’s a red flag.
What Triggers CRPS?
CRPS doesn’t come out of nowhere. It usually starts after trauma. The most common trigger? Fractures. About 40% of cases follow a broken bone-especially wrist fractures. Other triggers include surgery (like carpal tunnel repair or knee arthroscopy), sprains, cuts, burns, or even a cast that’s too tight.
Here’s the puzzle: many people break bones or have surgery and never get CRPS. Why do some people develop it and others don’t? Scientists think it’s a mix of factors: inflammation, nerve damage, immune system overreaction, and maybe even genetics. A 2022 study found autoantibodies in 30% of CRPS patients-meaning the body’s own immune system might be attacking its nerves.
It’s not always obvious. About 10% of cases develop without any clear injury. Some people report pain starting after a simple bump or even a blood draw. That’s why doctors now say CRPS isn’t always triggered by trauma-it’s triggered by the body’s abnormal response to it.
How Is It Diagnosed?
There’s no blood test or X-ray that confirms CRPS. Diagnosis relies on the Budapest Criteria-a set of signs and symptoms doctors use to spot it. You must have:
- Pain that’s disproportionate to any initial injury
- At least one symptom in three of these four categories: sensory (burning, tingling), vasomotor (temperature or color changes), sudomotor/edema (swelling, sweating), and motor/trophic (weakness, tremors, nail/hair changes)
- No other diagnosis that better explains your symptoms
Early diagnosis is critical. If caught within the first three months, treatment has the best chance of stopping it from becoming permanent. After six months, the condition often hardens. Nerves become more damaged, muscles atrophy, and the brain’s pain map rewires itself. That’s why so many people end up with lifelong pain-they weren’t diagnosed early enough.
Treatment: What Actually Works?
There’s no magic pill. But early, aggressive treatment can change the outcome. The goal isn’t just to numb the pain-it’s to retrain your nervous system.
Physical therapy is the most important step. Moving the affected limb-even if it hurts-is proven to reduce long-term disability. Graded motor imagery and mirror therapy are two specialized techniques that help your brain “unlearn” the pain signal. A 2021 study showed patients who did daily mirror therapy for 8 weeks improved movement and reduced pain by over 50%.
Medications help manage symptoms. NSAIDs like ibuprofen can reduce early inflammation. Corticosteroids are sometimes used in the first few weeks. For nerve pain, gabapentin, pregabalin, or amitriptyline are common. Ketamine infusions are being tested in clinics for severe cases. Some patients get nerve blocks-shots that temporarily interrupt pain signals. Spinal cord stimulators, which send mild electrical pulses to block pain, are used for chronic cases.
But drugs alone won’t fix it. CRPS needs a team: a pain specialist, a physiotherapist, a psychologist, and sometimes a neurologist. Mental health matters. Chronic pain changes how you think, sleep, and feel about yourself. Anxiety and depression aren’t just side effects-they make the pain worse.

What’s the Long-Term Outlook?
Some people recover fully. Others live with pain for years. About 50% of cases improve significantly within a year if treated early. But if it’s ignored for six months or more, the chance of full recovery drops sharply.
It’s not hopeless. Many people learn to manage it. They find ways to move, sleep better, and reduce stress. They stop fighting the pain and start working with their bodies. That shift-from victim to manager-is often the turning point.
Research is moving fast. Scientists are testing new drugs that target inflammation and autoimmunity. Wearable sensors are being developed to detect early signs before pain becomes unbearable. The hope is that one day, we’ll be able to predict who’s at risk and stop CRPS before it starts.
What Should You Do If You Suspect CRPS?
If you’ve had an injury and your pain isn’t fading-if it’s burning, spreading, or getting worse with light touch-don’t wait. Don’t assume it’s just “slow healing.” Go to your GP or a pain clinic. Bring a list of your symptoms: when they started, what makes them better or worse, how your skin looks and feels.
Ask: Could this be CRPS? Many doctors still don’t know about it. If they dismiss you, ask for a referral to a specialist in neuropathic pain. Early action saves limbs, sleep, and sanity.
CRPS doesn’t have to be a life sentence. But it demands attention-right now.
Is CRPS the same as regular nerve pain?
No. Regular nerve pain, like sciatica or diabetic neuropathy, usually follows a clear nerve pathway and stays in one area. CRPS is more complex-it involves inflammation, abnormal blood flow, skin changes, and movement problems. It’s not just a damaged nerve; it’s the whole nervous system going into overdrive.
Can CRPS spread to other parts of the body?
Yes. In about 70% of cases, the pain spreads beyond the original injury site. It might move up the limb or even affect the opposite side. This is called mirror-image spread. It’s not random-it’s a sign the brain’s pain processing is changing. Early treatment reduces this risk.
Does stress make CRPS worse?
Absolutely. Stress triggers the sympathetic nervous system, which is already overactive in CRPS. Anxiety, lack of sleep, or emotional trauma can spike pain levels. That’s why mindfulness, therapy, and pacing activities are part of treatment-not just extras.
Will a cast or splint cause CRPS?
Not directly. But if a cast is too tight, it can cut off circulation or put pressure on nerves, which may trigger CRPS in someone already at risk. That’s why doctors now check casts regularly and encourage movement as soon as possible.
Is CRPS permanent?
Not always. About half of people recover within a year with early treatment. But if it’s ignored for more than six months, the risk of long-term pain increases. Some people live with it for decades, but many learn to manage it well enough to work, drive, and live full lives.
Can children get CRPS?
Yes. Children make up about 5-10% of cases. They often recover faster than adults, especially with early physical therapy and family support. But it’s often misdiagnosed as “growing pains” or psychosomatic, leading to delays in treatment.
Are there any home remedies that help?
Not cures, but some things help manage symptoms. Gentle movement, warm baths (if your skin isn’t too sensitive), and stress-reducing techniques like deep breathing can help. Avoid ice or extreme heat on the affected area-it can worsen pain. Never stop prescribed therapy or meds without talking to your doctor.






Blow Job
December 24, 2025 AT 09:52Man, I had a wrist fracture last year and thought the burning was just part of healing. Turns out it was CRPS. No one took me seriously until I showed up with a doctor’s note and a thermal imaging printout. Don’t wait like I did.
Rachel Cericola
December 26, 2025 AT 04:39As someone who’s worked with chronic pain patients for over 15 years, I can’t stress this enough: CRPS isn’t ‘in your head’-it’s in your nerves, your immune system, and your brain’s wiring. I’ve seen patients go from bedridden to hiking again with mirror therapy and graded exposure. It’s not a cure, but it’s a lifeline. The biggest mistake? Waiting for the pain to ‘get worse’ before acting. Early intervention is everything. Physical therapy isn’t optional-it’s the frontline. And yes, your mental health is part of the treatment plan, not a side note. If your doctor doesn’t mention neuroplasticity or central sensitization, find someone who does. This isn’t about toughness. It’s about science.
Paula Villete
December 28, 2025 AT 03:39So… we’re telling people to ‘move through the fire’ while ignoring that some of us can’t even wear socks without screaming? Cool. Real helpful.
Gray Dedoiko
December 28, 2025 AT 23:41My sister had CRPS after a simple sprain. They told her it was anxiety. She cried every night for months. Then she found a pain clinic that actually listened. Now she does yoga and doesn’t need morphine. It’s not magic-it’s just being heard.
Andy Grace
December 30, 2025 AT 08:14Been there. Burned out three sets of physical therapists because I refused to believe I wasn’t just being dramatic. Took me a year to realize the pain wasn’t the enemy-it was the fear of it. Still not ‘fixed,’ but I don’t flinch at a breeze anymore.
John Pearce CP
December 30, 2025 AT 13:53It is a scientific fact that the modern healthcare system has become too soft. CRPS is not a disease of the body-it is a disease of the weak. If you cannot endure pain with stoicism, you should not be granted the title of ‘patient.’ The West has coddled illness into a lifestyle. This post is a symptom of the decline.
EMMANUEL EMEKAOGBOR
January 1, 2026 AT 06:50In Nigeria, we have a saying: ‘The fire that burns inside does not always have smoke.’ Many with CRPS are dismissed because their pain has no visible wound. I’ve seen elders treat such pain with herbal baths and community prayer-sometimes, the body heals when the mind feels held. Not a replacement for medicine, but a complement. We must not forget the human in the diagnosis.
CHETAN MANDLECHA
January 1, 2026 AT 15:00CRPS? Sounds like what my cousin got after a bike crash. Docs said it was ‘psychosomatic.’ Took him 3 years and a second opinion to get real help. Now he’s a disability advocate. Don’t let anyone tell you it’s ‘all in your head.’ Your pain is real, even if they don’t understand it.
niharika hardikar
January 3, 2026 AT 12:35It is imperative to note that the diagnostic criteria outlined herein, while clinically referenced, lack sufficient biomarker validation. The Budapest Criteria remain a heuristic construct, not a neurophysiological taxonomy. The conflation of autonomic dysregulation with central sensitization is methodologically unsound without fMRI or quantitative sensory testing. Until we establish a molecular signature, we risk pathologizing normal nociceptive variability.
Ajay Sangani
January 3, 2026 AT 23:50i mean… if the brain is just misreading signals… then is pain even real? or is it just the mind’s way of telling us we’re scared? like… if a tree falls in the forest and no one feels it… does the pain still exist? i think crps is less a disease and more a conversation between the body and the soul. and maybe the soul is just tired.
Pankaj Chaudhary IPS
January 5, 2026 AT 16:44As an officer who has worked with trauma survivors, I say this: resilience is not about enduring pain silently. It is about seeking help with dignity. CRPS is not weakness-it is a silent war fought daily by people who never asked for it. We must honor their courage with better systems, not silence. To the medical community: listen. To the patient: you are not alone.
Chris Buchanan
January 5, 2026 AT 17:23So let me get this straight: you’re telling me I should move my arm even though it feels like someone’s pouring acid on my skin… and that’s the ‘treatment’? Bro, I don’t need motivation-I need a time machine to undo the fracture.
Delilah Rose
January 6, 2026 AT 16:28I’ve lived with CRPS for 11 years. I’ve tried ketamine, spinal stimulators, acupuncture, CBD, hypnosis, and 17 different PTs. The only thing that made a real difference? My dog. He’d lie on my bad leg, and somehow, the burning would dull. Not because of science-because he didn’t care if I was in pain. He just loved me. Sometimes, healing isn’t about fixing the body. It’s about feeling safe enough to let it rest.
Georgia Brach
January 6, 2026 AT 21:07Let’s be honest: this post reads like a pharmaceutical marketing brochure. Who funded this? Who benefits from the ‘early intervention’ narrative? The pain industry thrives on chronicity. And yet, no one mentions that 80% of CRPS patients are women-coincidence? Or is this another example of medical gaslighting dressed up as compassion?