SSRI-Anticoagulant Risk Calculator
Personal Risk Assessment
Personalized Results
Important Note: This tool estimates risk based on published medical data. Always consult your doctor for personalized medical advice.
Combining SSRIs with anticoagulants is more common than you think. About 1 in 5 people on blood thinners also have depression or anxiety-and SSRIs are the go-to treatment. But here’s the problem: this combo increases your risk of serious bleeding. Not a little. Not rarely. SSRIs can make anticoagulants more dangerous by messing with your platelets, and the risk is highest in the first month.
Why This Combo Is Riskier Than It Looks
SSRIs like sertraline, escitalopram, and fluoxetine don’t just affect your mood. They also stop serotonin from getting into your platelets. Platelets need serotonin to stick together and form clots when you bleed. Without it, they’re slower to respond. Studies show this cuts platelet aggregation by 30-40%. That’s not a minor effect. It’s enough to turn a small cut into a serious bleed. When you add this to an anticoagulant-whether it’s warfarin, apixaban, or rivaroxaban-you’re stacking two things that thin your blood. One works on clotting factors. The other works on platelets. Together, they don’t just add up-they multiply. A 2024 study tracking over 42,000 people with atrial fibrillation found that those taking both an SSRI and an anticoagulant had a 33% higher chance of major bleeding than those on anticoagulants alone. That’s not theoretical. It means 6 extra bleeding events per 1,000 patients each year. Most of those were gastrointestinal bleeds-58% of cases. Others were brain bleeds or bleeding in other major organs.When Is the Risk Highest?
The danger isn’t steady. It spikes in the first 30 days after starting the SSRI. That’s when your platelets are adjusting to the sudden drop in serotonin. By six months, the risk drops significantly-likely because your body adapts, or doctors start monitoring more closely. But those first weeks? That’s when you need to be extra careful. This is why many experts say: if you’re starting an SSRI while already on a blood thinner, watch for signs of bleeding in the first month. Bruising that won’t fade. Dark, tarry stools. Nosebleeds that won’t stop. Headaches that feel different. These aren’t just side effects-they could be early warning signs.Not All Blood Thinners Are the Same
If you’re on warfarin, your risk is higher than if you’re on a DOAC like apixaban or rivaroxaban. The 2024 study showed a 28% increased bleeding risk with warfarin plus SSRI, compared to 22% with DOACs. That difference might seem small, but it matters-especially if you’re already at high risk for bleeding. Warfarin is harder to control. Its effects swing with diet, other meds, and even your liver function. Add an SSRI, and suddenly your INR can climb unexpectedly. That’s why doctors often check your INR twice a week for the first month if you start an SSRI while on warfarin. DOACs don’t need regular blood tests, but they still interact with SSRIs. The platelet effect doesn’t care what kind of anticoagulant you’re on. It’s the same mechanism. So even if you’re on a newer blood thinner, you’re not out of the woods.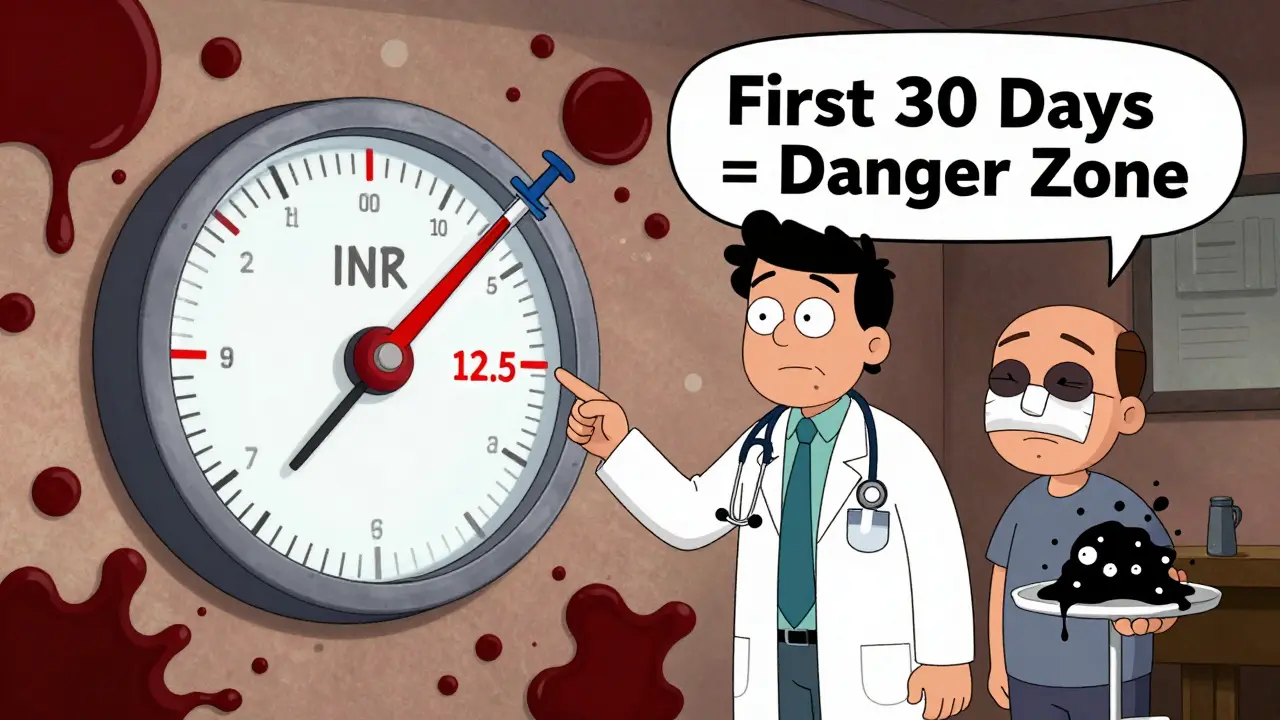
Are Some SSRIs Safer Than Others?
You might think the strongest SSRI-like paroxetine-would be riskiest. But the data says otherwise. The same 2024 study found no difference in bleeding risk between high-potency SSRIs (paroxetine) and lower-potency ones (escitalopram). Even though paroxetine blocks serotonin reuptake more aggressively, the bleeding outcome was identical. Sertraline is the most commonly prescribed SSRI in this group-used in over half of cases. Why? Not because it’s safer for bleeding, but because it has fewer interactions with other drugs. It doesn’t mess much with liver enzymes that break down anticoagulants. That makes it easier to manage in complex patients. So don’t assume switching from fluoxetine to sertraline will lower your bleeding risk. The platelet effect is the same across the board. The real difference comes from how the drug interacts with other medications-not how strong it is against serotonin.What About Other Antidepressants?
If you’re on a blood thinner and need help with depression, you have options that don’t touch platelets. Mirtazapine and bupropion are two that don’t interfere with serotonin uptake in platelets. Studies show they carry little to no added bleeding risk when paired with anticoagulants. The European Heart Rhythm Association recommends these as alternatives for patients with a high bleeding risk-especially if their HAS-BLED score is 3 or higher. That score looks at things like high blood pressure, kidney disease, age over 65, and past bleeding. If you’re on that list, switching from an SSRI might be the smartest move. But here’s the catch: SSRIs still work better for many people with moderate to severe depression. And they’re still the first choice in 87% of cases, according to 2023 prescription data. That’s because the benefits of treating depression-better sleep, less stress, improved heart health-often outweigh the bleeding risk, as long as you’re monitored.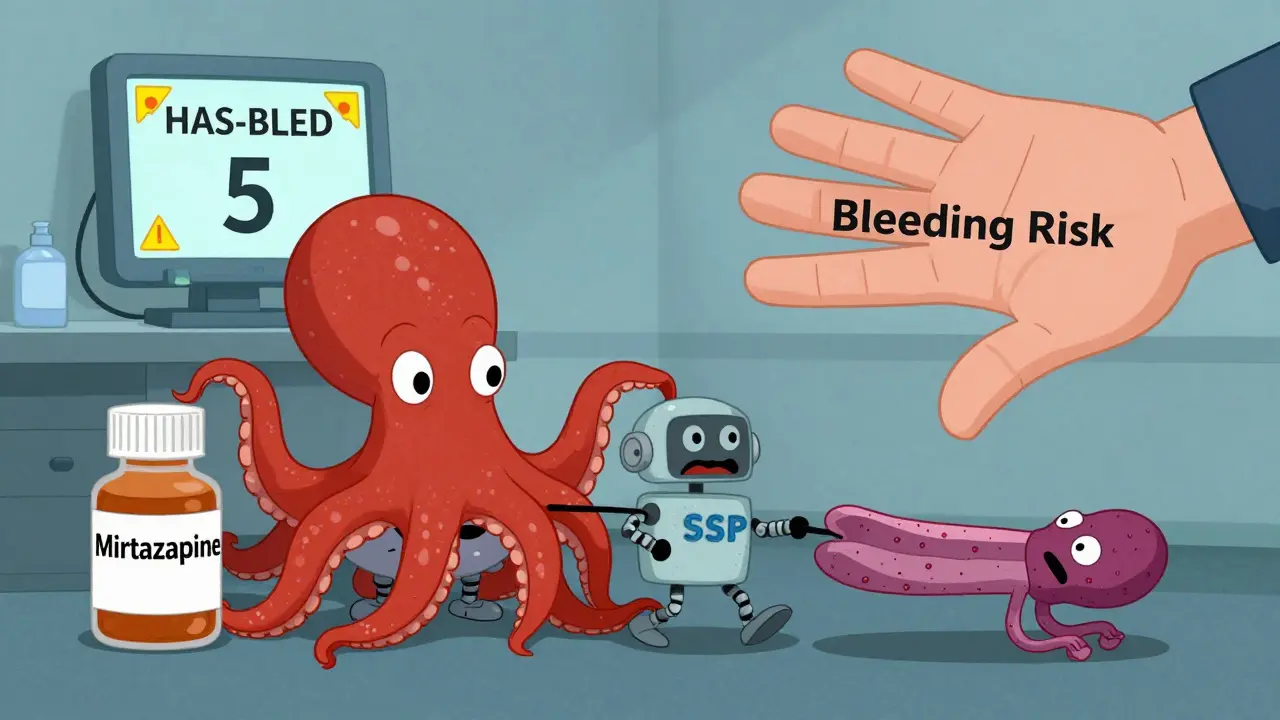
What Should You Do?
If you’re on an anticoagulant and your doctor suggests an SSRI, don’t panic. But do ask these questions:- Is this the best antidepressant for my bleeding risk?
- Will I need more frequent blood tests?
- What signs of bleeding should I watch for in the first month?
- Could I try mirtazapine or bupropion instead?
Monitoring and Prevention
If you’re on both drugs, you need a plan:- Baseline blood test: CBC and fecal occult blood test before starting the SSRI.
- Monthly checks for the first three months: Look for drops in hemoglobin or signs of hidden bleeding.
- For warfarin users: INR checked twice a week for the first month, then weekly for the next two months.
- Watch for bruising, gum bleeding, or dark stools. Report them immediately.
- Avoid NSAIDs like ibuprofen or naproxen. They add another layer of bleeding risk.





Dee Humprey
January 3, 2026 AT 22:45Just had my INR spike last month after starting sertraline. My cardiologist didn’t warn me. Learned the hard way. Now I get bloodwork every two weeks and avoid ibuprofen like the plague. Don’t assume your doctor knows this combo is risky-ask. Seriously.
Also, mirtazapine changed my life. No bleeding, no brain fog. If you’re on warfarin and depressed, it’s worth a try.
Michael Rudge
January 5, 2026 AT 00:22Oh wow. Another ‘medical advice’ post from someone who read a PubMed abstract and now thinks they’re Dr. House. SSRIs cause bleeding? Shocking. Next you’ll tell us oxygen causes fire.
Meanwhile, my 82-year-old grandma takes fluoxetine and apixaban and still hikes 5 miles a week. Maybe your ‘risk’ is just bad prescribing, not the drugs.
Stephen Craig
January 5, 2026 AT 06:14Two systems thinning blood-one pharmacological, one physiological. It’s not additive. It’s synergistic. The body doesn’t compartmentalize risk. It just bleeds.
Depression isn’t a choice. Neither is atrial fibrillation. But we can choose how we manage the overlap.
en Max
January 6, 2026 AT 14:52Per ACC/AHA 2024 guidelines, the HAS-BLED score should be recalibrated when initiating serotonergic agents in patients on DOACs, particularly if concomitant NSAID use or renal impairment (eGFR <60) is present. The platelet serotonin transporter inhibition is a Class IIa recommendation for monitoring.
Also, fecal occult blood testing is underutilized. Consider it mandatory in the first 30 days.
bob bob
January 8, 2026 AT 03:50I was on citalopram and rivaroxaban for 18 months. Never had a problem. But I did have weird bruising on my thighs after a fall-thought it was just aging. Turns out, it was the combo. Got switched to bupropion. Zero issues since.
Point is: listen to your body. And don’t be afraid to ask for a second opinion.
Clint Moser
January 9, 2026 AT 11:10They don't want you to know this but SSRIs are part of the pharma-anticoagulant complex designed to increase hospital admissions. The FDA knew. The studies were suppressed. 33% higher bleed risk? That's just the tip. They're using your depression to sell more warfarin tests.
Also, DOACs are made by Big Pharma to replace warfarin so they can charge $500/month. Same thing. Different label.
Roshan Aryal
January 9, 2026 AT 21:45America again, treating depression like a glitch to be patched with chemicals while ignoring root causes. In India, we use yoga, sunlight, and community. No pills. No bleeding. No $1.2 billion waste.
You people medicate your loneliness. Then wonder why you’re always bruising.
Jennifer Glass
January 10, 2026 AT 11:11This is so well-written. I’m a nurse and I’ve seen this happen twice in my unit. One guy had a GI bleed after starting escitalopram. No one asked if he was on anticoagulants. He almost died.
Doctors need better alerts. Patients need better education. This isn’t rare. It’s systemic.
Angie Rehe
January 10, 2026 AT 12:38WHY IS NO ONE TALKING ABOUT THE FACT THAT SSRIs ARE DESIGNED TO DEPLETE SEROTONIN IN PLATELETS? THIS ISN’T AN ACCIDENT. IT’S A FEATURE. THEY WANT YOU BLEEDING SO YOU COME BACK FOR MORE TESTS AND MORE DRUGS.
THEY’RE PROFITING OFF YOUR FEAR. STOP TRUSTING THE SYSTEM.
melissa cucic
January 11, 2026 AT 09:13I appreciate the depth of this post. The 2024 study’s findings are critical-and yet, still under-discussed in primary care. The fact that paroxetine and escitalopram show equivalent bleeding risk despite differing potency suggests that the mechanism is class-wide, not agent-specific.
Also, the emphasis on the first 30 days is spot-on. That’s the window where vigilance must be non-negotiable. I’ve shared this with my entire clinic’s continuing education group.
And yes-mirtazapine is a viable alternative, especially for patients with high HAS-BLED scores. It’s underutilized because it causes weight gain. But sometimes, safety trumps aesthetics.
Justin Lowans
January 13, 2026 AT 05:27This is the kind of post that reminds me why I still believe in thoughtful medical discourse. Too often, we reduce complex conditions to soundbites.
But here? We have data, nuance, and actionable advice. The fact that bleeding risk drops after six months suggests neuroadaptation-not just monitoring. That’s worth exploring further.
And yes, we need better tools. I’ve started using a simple checklist in my practice: SSRI? Anticoagulant? HAS-BLED ≥3? → Consider mirtazapine or bupropion. It’s saved at least three patients from avoidable bleeds.
Thank you for writing this.
Akshaya Gandra _ Student - EastCaryMS
January 14, 2026 AT 07:51can u explain what is DOAC again? im student and dont get it
Jennifer Glass
January 14, 2026 AT 10:50DOAC = Direct Oral Anticoagulant. Think apixaban, rivaroxaban, dabigatran. Newer blood thinners that don’t need weekly blood tests like warfarin. They’re easier to use but still interact with SSRIs the same way.
Hope that helps 😊
mark etang
January 15, 2026 AT 23:37It is imperative to underscore that the concomitant administration of selective serotonin reuptake inhibitors with anticoagulant agents constitutes a pharmacodynamic interaction of significant clinical consequence. The resultant impairment of platelet aggregation, compounded by the inhibition of coagulation cascade proteins, creates a state of heightened hemostatic vulnerability.
As such, the implementation of a multidisciplinary risk mitigation protocol-including baseline hematologic assessment, structured patient education, and mandatory follow-up intervals-is not merely advisable-it is a standard of care.
Jack Wernet
January 17, 2026 AT 00:23I’m from a small town in Nebraska. Our local clinic doesn’t have a psychiatrist. My GP prescribed sertraline while I was on Xarelto. I didn’t know to ask. Two weeks later, I passed out from anemia.
Thank you for this. I’m sharing it with everyone I know who’s on blood thinners. We need to stop assuming doctors know everything.