When your skin starts burning, itching, or flaking after using a cream or ointment, it’s easy to blame the condition you’re trying to treat-eczema, psoriasis, a rash. But what if the treatment itself is the problem? Topical medication allergies are more common than most people realize, and they often get missed because doctors assume the medicine can’t cause the reaction it’s meant to fix.
What Is Contact Dermatitis?
Contact dermatitis is a red, itchy, sometimes blistering rash that shows up where your skin touched something irritating or allergenic. There are two types: irritant and allergic. Irritant contact dermatitis happens when a substance like soap, bleach, or even excessive handwashing damages your skin’s outer layer. It’s not an immune response-it’s physical wear and tear.
Allergic contact dermatitis is different. It’s your immune system reacting to a specific chemical you’ve been exposed to before. This is the kind tied to topical medications. It doesn’t happen the first time you use a cream. It takes repeated exposure for your body to recognize the substance as a threat. Then, days later, your skin breaks out.
Think of it like a silent alarm. You’ve used hydrocortisone cream for months. One day, the rash gets worse instead of better. Your skin feels hotter. It itches more. You might even see tiny blisters. That’s not the eczema flaring up-it’s your body saying, “I’ve had enough of this.”
Which Medications Cause Allergic Reactions?
Over 360 drugs have been linked to allergic contact dermatitis. But a few stand out as the usual suspects. Antibiotics top the list. Neomycin, found in many over-the-counter ointments like Neosporin, triggers reactions in nearly 1 in 10 people tested. Bacitracin and gentamicin are close behind.
Corticosteroids-often the go-to treatment for skin inflammation-are also common offenders. About 0.5% to 2.2% of people using them develop an allergy to the very drug meant to help. That creates a cruel loop: you apply hydrocortisone to calm your skin, but your immune system starts attacking it instead.
Local anesthetics like benzocaine (common in numbing creams and teething gels) and NSAIDs like ketoprofen (used in topical pain relievers) are also frequent triggers. Even preservatives and fragrances added to these medications can set off reactions.
Here’s the twist: you might be allergic to a medication you’ve never used. Cross-reactivity means if you’re sensitive to one steroid, you might react to others in the same chemical family. For example, if you’re allergic to hydrocortisone (Group A), you’re usually safe with triamcinolone (Group B) or methylprednisolone (Group D). Knowing these groups helps doctors pick alternatives without guessing.
Why Is It So Often Missed?
Doctors don’t always think to test for it. A 2023 review in Dermatology Times found that 40% to 60% of topical medication allergies are misdiagnosed at first. Why? Because the reaction looks like the original condition getting worse. If you have eczema and your cream makes it itchier, the assumption is: “It’s not working.” Not: “You’re allergic to it.”
Patients contribute too. Many don’t realize that their “natural” moisturizer, herbal salve, or even their partner’s sunscreen could contain allergens. One study found that 30% of allergic triggers come from products patients didn’t even consider “medications.”
Healthcare workers are especially at risk. About 18% of nurses and doctors develop contact dermatitis from topical meds they handle daily. A 2022 JAMA Dermatology study showed that over half of these cases needed workplace changes-like switching gloves or avoiding certain creams-because the problem kept coming back.
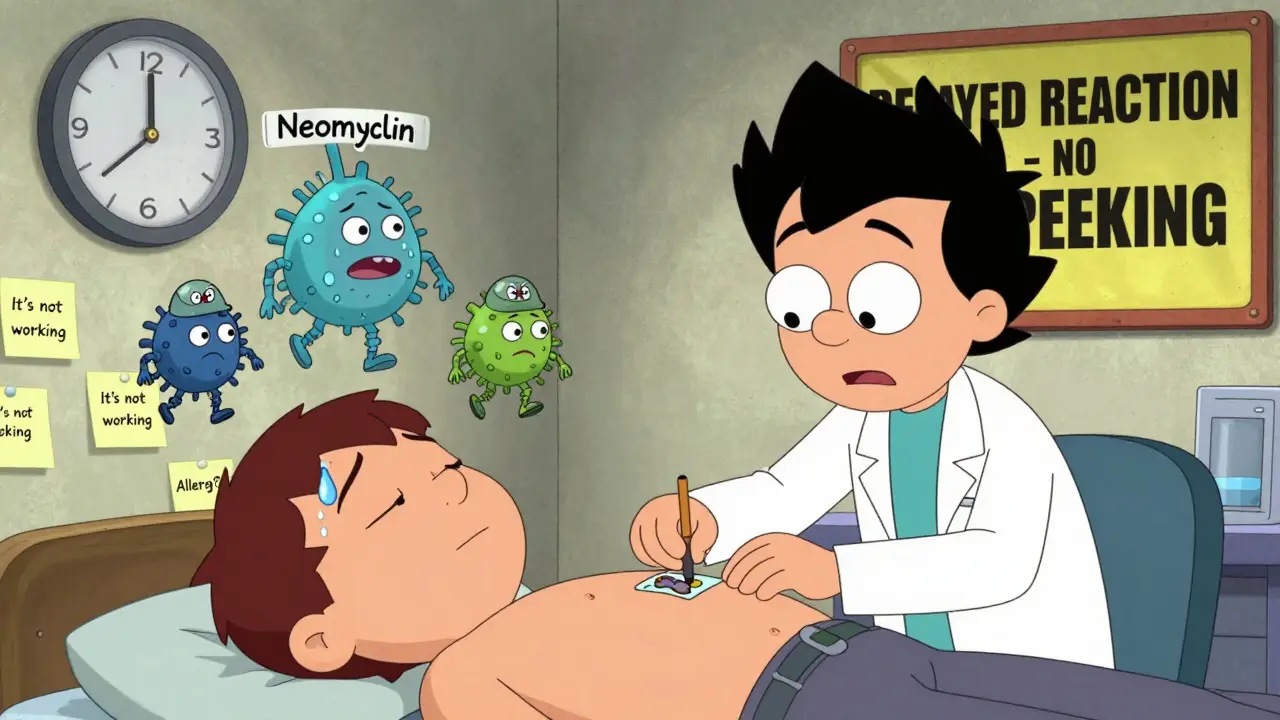
How Is It Diagnosed?
The gold standard is patch testing. It’s not a quick prick like a peanut allergy test. You wear small patches with potential allergens on your back for 48 hours. Then, your doctor checks for reactions at 48 and 96 hours. Why wait? Because allergic contact dermatitis is a delayed reaction-your T-cells need time to show up and cause inflammation.
When done right, patch testing finds the cause in about 70% of cases. But it’s not perfect. Skin that’s already damaged or inflamed can give false negatives. New research from Johns Hopkins shows that diluting the medication 10 times before testing helps catch allergies in people with broken skin barriers-cutting false negatives from 32% to just 9%.
There’s also a new tool: the Topical Medication Allergy Score, introduced in Europe in 2023. It uses 12 clinical clues-like how long the rash lasted, where it appeared, and whether it got worse after reapplying the cream-to predict allergy likelihood. With this score, diagnosis accuracy jumped from 65% to 89%.
How Is It Treated?
First and most important: stop using the allergen. That’s it. No fancy drugs. No miracle creams. Just avoidance. Studies show that 89% of chronic cases clear up within four weeks once the trigger is removed. Without that step, even the strongest steroids won’t help.
For mild cases, over-the-counter 1% hydrocortisone can help calm the itch. But if it’s not better in a week, you need a prescription. For moderate cases, doctors often prescribe mid- to high-potency steroids like triamcinolone 0.1% or clobetasol 0.05%. But here’s the catch: if the rash is on your face, eyelids, or groin, use low-potency options like desonide instead. High-potency steroids on thin skin can cause atrophy-thinning and wrinkling-seen in up to 35% of long-term users.
For large areas (over 20% of your body), you’ll need oral steroids like prednisone. A 2- to 3-week course, tapered slowly, brings relief in 85% of severe cases within a day or two.
When steroids aren’t an option-or when you’ve had too many-topical calcineurin inhibitors like pimecrolimus (Elidel) or tacrolimus (Protopic) are strong alternatives. They work well, with 60-70% of patients seeing improvement. But they can burn at first. One RealSelf survey found 41% of users felt a stinging sensation, though it faded after a few days.
And yes, you can still use steroids-just not the ones you’re allergic to. Knowing steroid groups lets doctors swap in safe ones. A patient allergic to hydrocortisone can often use mometasone or fluticasone without issue.

What to Do Next
If you suspect a topical medication allergy:
- Stop using the product immediately.
- Write down every cream, ointment, lotion, or spray you’ve used in the last 6 months-including makeup, sunscreen, and hand sanitizer.
- Bring all your products to your dermatologist. Don’t assume only prescriptions count.
- Ask for patch testing. It’s not routine, but it’s necessary if your rash won’t heal.
- Use the American Contact Dermatitis Society’s mobile app to scan products for allergens. It’s used by over 40% of patch-tested patients.
There’s also new hope on the horizon. Researchers are testing barrier creams that block allergens from penetrating the skin-early trials show a 73% reduction in exposure. And the NIH has funded $4.7 million to develop a blood test that could predict allergy risk before you even apply the cream.
Bottom Line
Topical medication allergies aren’t rare. They’re hidden. And they’re often mistaken for treatment failure. If your skin isn’t improving-or is getting worse-after using a cream, don’t assume it’s just not strong enough. Ask: Could this be the problem?
Stopping the allergen is the most powerful treatment you have. Patch testing gives you the answer. And once you know what to avoid, your skin can heal-without more creams, more side effects, or more frustration.
Can you be allergic to hydrocortisone cream?
Yes. Hydrocortisone is one of the most common causes of topical medication allergies. About 1 in 10 people who get patch tested for skin rashes test positive for hydrocortisone allergy. It’s ironic because it’s often used to treat rashes. If your rash gets worse after using it, that’s a red flag.
How long does contact dermatitis take to go away?
Once you stop using the allergen, itching usually improves within 48 to 72 hours. The rash itself can take 2 to 4 weeks to fully clear. If you keep using the trigger, it can become chronic-lasting months or longer. That’s why identifying the cause is so critical.
Is patch testing painful?
No. Patch testing involves small metal discs taped to your back. You don’t feel anything during the 48-hour wait. You might feel mild itching or burning if you react, but it’s not painful. The only discomfort is the inconvenience of not showering or sweating for two days.
Can I use Neosporin if I have sensitive skin?
Not if you’ve had unexplained rashes after using it. Neosporin contains neomycin, which causes allergic reactions in nearly 10% of patch-tested patients. Even if you’ve used it safely before, allergies can develop over time. For sensitive skin, plain petrolatum (Vaseline) or fragrance-free moisturizers are safer.
Are natural or organic topical products safer?
No. Many natural products contain plant extracts like tea tree oil, lanolin, or balsam of Peru-all common allergens. In fact, 30% of allergic triggers come from products people think are “safe” because they’re labeled natural or organic. Ingredients matter more than marketing claims.




Emma Duquemin
December 29, 2025 AT 13:09Okay but can we talk about how insane it is that we slap neomycin on cuts like it’s glitter? I had a tiny scrape and used Neosporin for weeks-turned out I was allergic. My skin looked like a dragon’s nest. No one warned me. Not even the pharmacist. Now I just use Vaseline and call it a day. 🤯
Kevin Lopez
December 30, 2025 AT 22:58Topical steroid allergy is underdiagnosed due to delayed-type hypersensitivity (Type IV) mechanisms. Patch testing remains gold standard, but clinical suspicion must precede testing. 1% hydrocortisone is not inert-it’s a haptens carrier. Cross-reactivity within Group A steroids is >80%. Stop treating symptoms-identify the sensitizer.
Duncan Careless
January 1, 2026 AT 08:22Just wanted to say thanks for writing this. I’ve been dealing with this for years and thought I was just ‘super sensitive.’ Didn’t realize it could be the meds themselves. Patch test next week. Fingers crossed.
Samar Khan
January 1, 2026 AT 10:25OMG I’m literally crying rn 😭 I’ve been using that ‘natural’ tea tree oil cream for my eczema for 2 years and now I find out it’s the reason my face looks like a pizza? I feel so stupid. Why didn’t anyone tell me?! 😭
Russell Thomas
January 2, 2026 AT 21:46So let me get this straight-you’re telling me the ‘miracle cream’ I’ve been slathering on for a decade is the reason my skin looks like a crime scene? And now you want me to stop? What’s next? Are you gonna tell me water causes acne too? 😒
Nicole K.
January 3, 2026 AT 10:34This is why people shouldn’t use random creams. If you don’t know what’s in it, don’t put it on your skin. It’s basic hygiene. I told my cousin this and she still uses lavender lotion. She’s got a rash that won’t go away. It’s her own fault.
Jasmine Yule
January 5, 2026 AT 03:53Thank you for this. I’ve been so frustrated trying to fix my skin while using the exact things meant to help. I just stopped everything for a week and my skin started healing. I didn’t realize how much I’d been blaming myself. This post felt like a hug.
Alex Ronald
January 5, 2026 AT 13:20Same here. I thought I was just bad at managing my eczema. Turns out I was allergic to the steroid cream my dermatologist prescribed. Switched to tacrolimus-burned like hell day one, but now my skin’s clear. Worth it. You’re not broken. It’s just the wrong cream.
Teresa Rodriguez leon
January 6, 2026 AT 15:32Ugh. I’ve been through this. My dermatologist laughed when I asked about patch testing. Said ‘it’s probably just stress.’ Two years later, I found out I was allergic to bacitracin in my daily hand cream. I wish I’d known sooner.
Manan Pandya
January 8, 2026 AT 08:33Interesting point about cross-reactivity. In India, we often use Ayurvedic pastes with balsam of Peru-common allergen. Many patients come with chronic rashes and no idea why. Education gap is massive here. This article should be translated.
Nisha Marwaha
January 9, 2026 AT 23:58Topical calcineurin inhibitors have a high rate of initial burning due to TRPV1 receptor activation-this is well-documented in JID 2021. Patients often discontinue prematurely. Pre-cooling the skin and applying a thin layer reduces discomfort by 60%. Pro tip: refrigerate before use.
Paige Shipe
January 10, 2026 AT 19:30So you’re saying I’m allergic to my own skin cream? And now I have to stop using my ‘natural’ stuff? I don’t believe this. I’m not some lab rat. My grandma used coconut oil for everything and lived to 92. This is just corporate fear-mongering.
Tamar Dunlop
January 12, 2026 AT 11:23As a Canadian nurse who has treated countless cases of occupational contact dermatitis, I can attest to the profound under-recognition of this issue in clinical practice. The emotional toll on patients is immense. Thank you for articulating this with such clarity and compassion.
David Chase
January 12, 2026 AT 13:58AMERICA NEEDS TO STOP LETTING PEOPLE SLATHER CHEMICALS ON THEIR SKIN LIKE THEY’RE DANCING AT A RAVE!!! 🇺🇸🔥 WHY ISN’T THIS A FEDERAL LAW?! I’M SICK OF PEOPLE DYING BECAUSE THEY USE ‘NATURAL’ SHIT THAT’S WORSE THAN ASBESTOS!!!
Greg Quinn
January 13, 2026 AT 03:15It’s funny how we treat our skin like a puzzle to solve with more products. We stack creams, oils, serums, toners-like we’re building a tower of hope. But sometimes, the answer isn’t another layer. It’s silence. Just stop. Let the skin breathe. Let it remember what it feels like to be untouched. Sometimes, healing is just not doing anything.