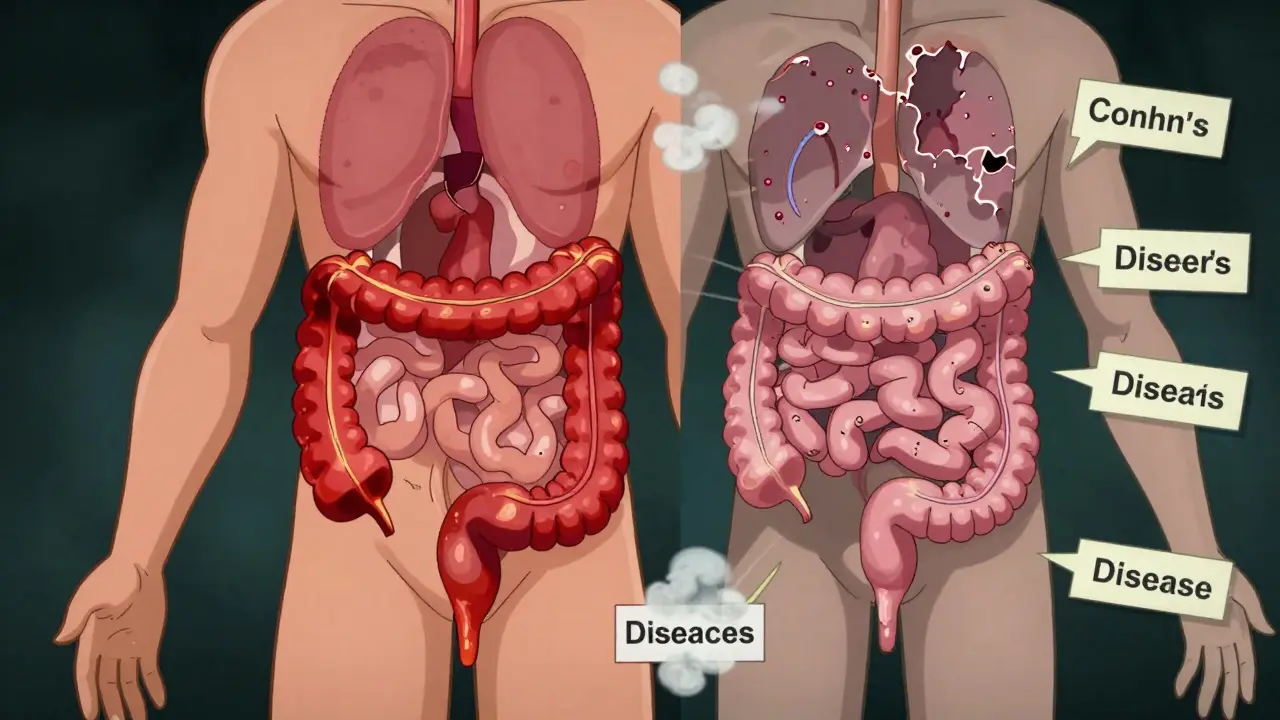
When someone hears "inflammatory bowel disease," they might think it’s one condition. But it’s not. It’s two very different diseases that look similar on the surface - but behave in completely different ways under the skin. Crohn’s disease and ulcerative colitis (UC) both cause painful inflammation in the digestive tract, lead to frequent bathroom trips, and can leave you exhausted. Yet, if you have one, your body is fighting a battle that’s fundamentally different from the other. And knowing which one you have changes everything - from what treatments work, to what complications you might face, to how you manage your life day to day.
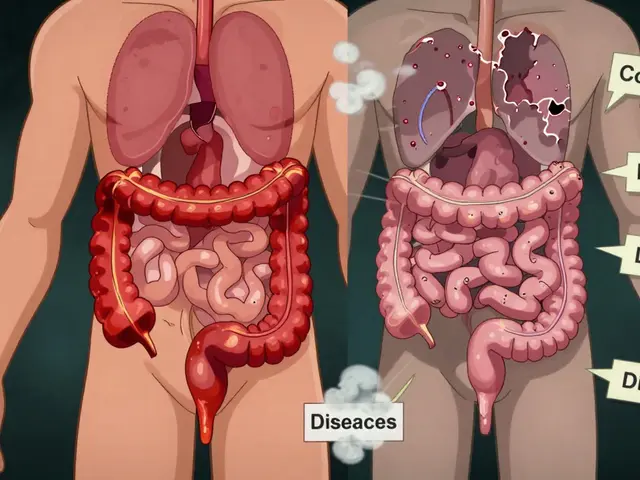
Where the Inflammation Lives
- Ulcerative colitis sticks to one place: the colon and rectum. It starts at the rectum and creeps upward, always in a continuous line. There’s no skipping. No gaps. If you have UC, the inflammation doesn’t jump around - it moves like a tide, covering the inner lining of your large intestine.
- Crohn’s disease doesn’t care where it shows up. It can hit anywhere from your mouth to your anus. Most often, it lands in the last part of the small intestine (the terminal ileum) or the beginning of the colon. But it can also appear in patches, leaving healthy tissue between inflamed areas. This is called "skip lesions," and it’s a dead giveaway for Crohn’s.
This difference isn’t just academic. It affects how doctors look for it. A colonoscopy for UC will show a red, raw, continuous line of damage starting at the rectum. For Crohn’s, you might see patchy ulcers, deep cracks in the lining, or a "cobblestone" appearance - like the surface of a rocky road. And because Crohn’s can affect the small intestine, you might need an MRI or capsule endoscopy (a pill-sized camera you swallow) to see what’s going on beyond the colon.
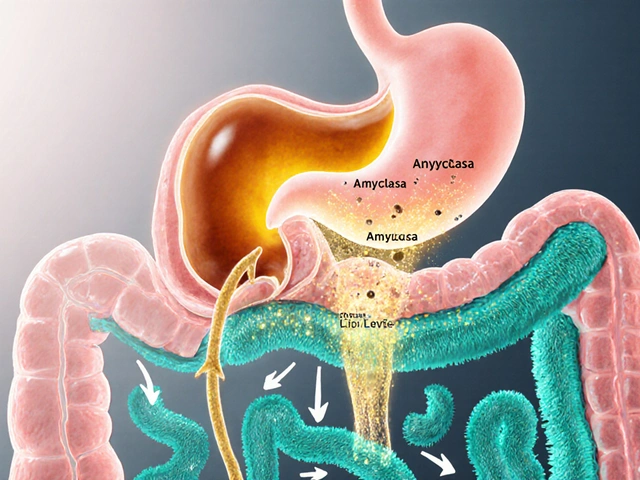
How Deep the Damage Goes
Ulcerative colitis stays shallow. It only eats away at the innermost layers of the bowel wall - the mucosa and submucosa. Think of it like a sunburn on your skin. It hurts, it bleeds, but it doesn’t go deep.
Crohn’s disease? It goes all the way through. It’s transmural. That means it burns through every layer - from the inside lining, past the muscle, and out to the outer membrane. This is why Crohn’s patients are at risk for things UC patients rarely see: fistulas and strictures.
- Fistulas are abnormal tunnels between parts of the bowel, or between the bowel and skin, bladder, or vagina. About 25% of people with Crohn’s will develop one in their lifetime. They can leak, get infected, and need surgery.
- Strictures happen when scar tissue builds up and narrows the intestine. Around one-third of Crohn’s patients develop them. Food or stool gets stuck. You feel bloated. You vomit. It’s a medical emergency.
These complications are rare in ulcerative colitis. Less than 5% of UC patients ever get a fistula. But UC has its own scary risk: toxic megacolon. That’s when the colon swells dangerously, loses muscle tone, and can rupture. It happens in about 5% of severe UC flares - and it’s life-threatening. You need surgery fast.
What the Blood and Stool Tests Tell You
There’s no single test that says "yes, this is Crohn’s" or "this is UC." But doctors use clues.
- Fecal calprotectin - a protein in stool that shows inflammation - is high in both, but tends to be higher in UC. Over 80% of active UC cases show levels above 250 μg/g.
- pANCA antibodies - a type of immune marker - show up in 60-70% of UC patients, but only 10-15% of Crohn’s patients. It’s not perfect, but it’s a strong hint.
- Crohn’s-specific markers like ASCA antibodies show up in 50-60% of Crohn’s cases, but rarely in UC. When both pANCA and ASCA are tested together, they help separate the two in about 80% of cases.
Doctors also look at how you respond to treatment. If you’re on a rectal enema and it works wonders? That’s more likely UC. If you need a pill that works systemically - something that affects your whole body - that’s more typical of Crohn’s.
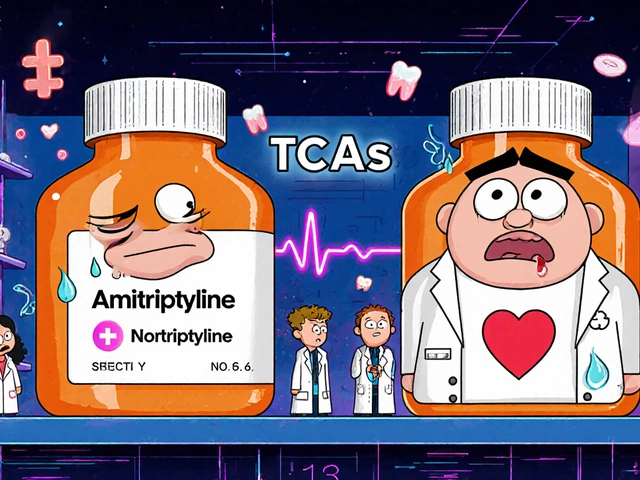
How Treatment Changes Based on the Disease
Both conditions use anti-inflammatories, immune suppressors, and biologics - but how they’re used differs.
- For ulcerative colitis: 5-ASAs (like mesalamine) in enema or suppository form are often the first step. They deliver medicine right where it’s needed - the colon. For mild to moderate cases, this puts about 60-80% of people into remission. If that fails, biologics like vedolizumab (which targets gut-specific immune cells) are very effective.
- For Crohn’s disease: Because it’s deeper and wider, you need drugs that work systemically. Azathioprine, methotrexate, or biologics like adalimumab (Humira) or infliximab (Remicade) are common. Anti-TNF drugs work better in Crohn’s - about 30-40% of patients go into remission at 54 weeks, compared to 20-30% in UC.
And then there’s surgery.
- UC: Removing the entire colon and rectum (proctocolectomy) is a cure. Afterward, many people get a pouch built from the small intestine - so they still go to the bathroom normally. About 10-15% of UC patients eventually need this.
- Crohn’s: Surgery removes the damaged part of the intestine - but it doesn’t cure anything. The disease always comes back, often right next to the surgical site. Half of Crohn’s patients need a second surgery within 10 years.
What Happens Outside the Gut
Both diseases can cause problems elsewhere. About one in three people with IBD gets something called an extraintestinal manifestation (EIM).
- Joint pain - swollen knees or fingers - affects 20% of both groups.
- Skin rashes like erythema nodosum (red, tender bumps on the shins) show up in 10-15%.
- Eyes - redness, pain, blurred vision - happen in 5-10%.
But there’s a key difference: primary sclerosing cholangitis (PSC), a serious liver disease that scars the bile ducts, is strongly tied to UC. About 3-7% of UC patients develop it. In Crohn’s? Only 0.5-1%. If you have UC and your liver enzymes are off, your doctor will check for PSC.
What Patients Say - Real Life Differences
Online forums and patient surveys show how these diseases feel in real life.
- People with UC report urgency - the sudden, uncontrollable need to go - far more often than Crohn’s patients. About 87% say it’s their biggest issue.
- Rectal bleeding is common in UC (75%) but rare in Crohn’s (35%).
- Crohn’s patients are more likely to struggle with nutritional problems. Because the small intestine is often affected, they can’t absorb vitamins, iron, or B12. Weight loss and fatigue are more common.
- On Reddit’s IBD community, UC patients say stress triggers their flares. Crohn’s patients point to specific foods - dairy, high-fiber veggies, or greasy meals.

The Uncertain Cases
Not everyone fits neatly into one box. About 10-15% of people are diagnosed with "indeterminate colitis" - meaning doctors can’t tell if it’s Crohn’s or UC at first.
And it gets weirder: 12% of people initially diagnosed with UC are later reclassified as having Crohn’s after a few years - because they develop fistulas, strictures, or inflammation outside the colon.
That’s why doctors don’t rely on one test. They watch. They recheck. They look at how you respond over time. Your diagnosis might change - and that’s okay.
What’s Next for Treatment
There’s new hope on the horizon.
- Fecal microbiota transplants (FMT) - basically, giving someone healthy gut bacteria - helped 32% of UC patients reach remission in a recent trial. But only 22% of Crohn’s patients responded. That tells us the gut microbiome plays a different role in each disease.
- New biologics like mirikizumab (for Crohn’s) and etrolizumab (for UC) are in late-stage trials. FDA decisions are expected by late 2024.
One thing’s clear: we’re moving beyond one-size-fits-all treatment. The future is personalized - based on where the disease lives, how deep it goes, and what your body responds to.
Cost and Burden
IBD isn’t just physically draining - it’s expensive.
- Severe ulcerative colitis costs about $38,451 per year in the U.S.
- Severe Crohn’s? Around $38,451 - similar, but often higher due to more surgeries and complications.
And it’s getting worse. IBD rates are rising in newly industrialized countries - likely due to diet, hygiene, and environmental changes. In the UK, about 1 in 200 people live with IBD. In Manchester, that’s tens of thousands.
Can you have both Crohn’s disease and ulcerative colitis at the same time?
No, you can’t have both at the same time. They’re two distinct diseases. But sometimes, it’s hard to tell which one you have at first - especially if inflammation is limited to the colon. That’s called indeterminate colitis. Over time, as symptoms or complications develop, doctors can usually reclassify it as one or the other. About 12% of people initially diagnosed with UC later turn out to have Crohn’s.
Does stress cause IBD?
No, stress doesn’t cause Crohn’s or ulcerative colitis. These are autoimmune diseases triggered by genetics and environmental factors - like diet, antibiotics, or the gut microbiome. But stress can make symptoms worse. Many patients report flares after major life events. Managing stress doesn’t cure IBD, but it helps keep things stable.
Is IBD the same as IBS?
No. IBS (Irritable Bowel Syndrome) is a functional disorder - meaning the gut looks normal but doesn’t work right. It causes bloating, cramps, and changes in bowel habits, but no inflammation, no bleeding, and no damage to the tissue. IBD involves real, visible inflammation that can lead to ulcers, scarring, and even cancer. They’re often confused, but they’re completely different.
Can you outgrow IBD?
No. IBD is a lifelong condition. You can go into remission - sometimes for years - with the right treatment. But the disease doesn’t disappear. Even if you feel fine, the inflammation may still be there under the surface. That’s why regular check-ups and monitoring are essential.
Does diet cure IBD?
No diet can cure Crohn’s or ulcerative colitis. But what you eat can help manage symptoms. Some people find relief by avoiding dairy, high-fiber foods, or spicy meals. Others benefit from low-FODMAP diets. But these are tools for symptom control - not cures. Always work with a dietitian who knows IBD. Starving yourself or cutting out entire food groups can lead to malnutrition, which makes things worse.
If you’ve been diagnosed with IBD, know this: you’re not alone. Whether it’s Crohn’s or UC, your journey is unique. But the tools to manage it - from medication to diet to surgery - are better than ever. And the more you understand the difference between these two diseases, the better you can work with your doctor to take control.



Scott Conner
February 9, 2026 AT 12:07Random Guy
February 10, 2026 AT 04:03Tasha Lake
February 11, 2026 AT 21:43Alex Ogle
February 12, 2026 AT 09:41Brett Pouser
February 12, 2026 AT 21:02Simon Critchley
February 13, 2026 AT 11:23Tom Forwood
February 14, 2026 AT 10:20Karianne Jackson
February 14, 2026 AT 11:25Tori Thenazi
February 16, 2026 AT 01:58Elan Ricarte
February 17, 2026 AT 11:19Angie Datuin
February 19, 2026 AT 08:24Andrew Jackson
February 19, 2026 AT 10:40Camille Hall
February 20, 2026 AT 08:27Ryan Vargas
February 20, 2026 AT 23:44