If you wake up tired even after eight hours in bed, your sleep position might be the culprit. For many people with obstructive sleep apnea, sleeping on their back isn’t just uncomfortable-it’s dangerous. The difference between sleeping on your back versus your side can mean the difference between 30 breathing pauses an hour and fewer than five. This isn’t speculation. It’s backed by sleep labs and clinical studies. Positional therapy, which trains you to avoid sleeping on your back, is one of the most underused but effective tools for managing sleep apnea-especially if your apnea gets worse when you’re on your back.
Why Sleeping on Your Back Makes Apnea Worse
When you lie on your back, gravity pulls your tongue and soft tissues in your throat backward. This narrows your airway by 30-40%, making it far easier for it to collapse during sleep. In clinical terms, this is called positional obstructive sleep apnea (POSA). It’s diagnosed when your apnea-hypopnea index (AHI)-the number of breathing pauses per hour-is at least twice as high when you’re on your back compared to when you’re on your side.Studies show that 50-60% of people with sleep apnea have POSA. For some, it’s even higher. One sleep study found that patients with POSA had significantly longer apnea events, deeper oxygen drops, and more heart rate spikes when sleeping supine. These aren’t minor inconveniences. They’re stressors on your heart, brain, and metabolism. And they happen every night, quietly, while you think you’re sleeping.
Side Sleeping: The Natural Fix
Sleeping on your side keeps your airway open. There’s no gravity pulling your tongue backward. Your throat stays more open. Snoring drops. Breathing improves. Oxygen levels stabilize. The Sleep Foundation calls side sleeping the best position for sleep apnea-and for good reason.Many patients report immediate results. Bed partners often notice snoring stops within seconds of a person rolls onto their side. One study found that positional therapy reduced the supine AHI by an average of 7.5 events per hour. That’s not a small gain-it’s the difference between moderate and mild apnea. For some, it’s enough to eliminate the need for CPAP entirely.
Positional Therapy: What Works and What Doesn’t
Positional therapy isn’t just about wanting to sleep on your side. It’s about training your body to stay there. There are two main approaches: simple, low-cost methods and advanced devices.The classic tennis ball technique-sewing a tennis ball into the back of a t-shirt-is cheap and widely recommended. But it’s not always comfortable. About 45% of people who try it quit within three months because it hurts, disrupts sleep, or just feels awkward. It works, but it’s not sustainable for most.
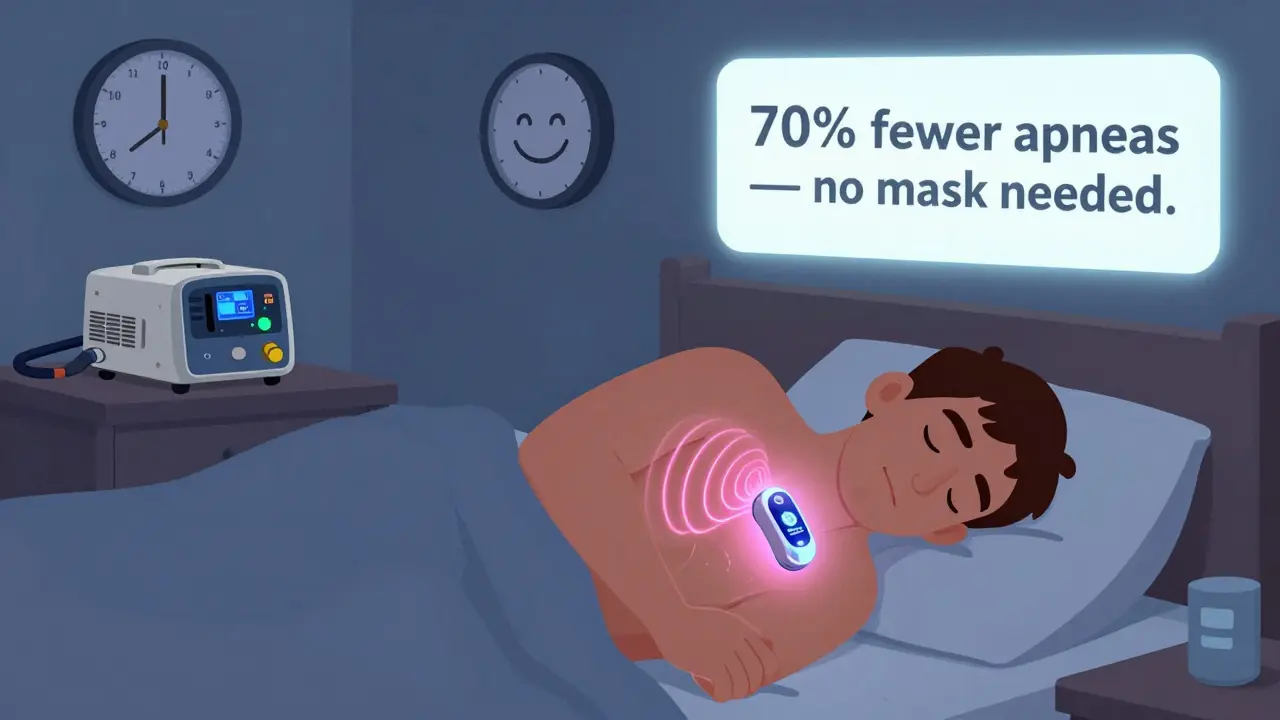
More advanced tools like the Sleep Position Trainer (SPT) use gentle vibrations to nudge you back to your side when you roll onto your back. These devices don’t wake you up-they just remind you. A 2015 study in the Journal of Clinical Sleep Medicine found that SPT reduced supine sleeping to 0% for most users. More importantly, 68% of SPT users reached treatment success (AHI under 5), compared to just 43% with the tennis ball method. Users also reported better sleep quality and higher satisfaction.
Other devices like Smart Nora use subtle air movement to open the airway when snoring starts, but they’re not true positional therapy. They treat the symptom, not the cause. SPT and similar wearables target the root problem: sleeping on your back.

How It Compares to CPAP
CPAP is the gold standard. It works. But it’s hard to stick with. Long-term adherence rates hover around 50-60%. Many people quit because the mask is uncomfortable, the machine is noisy, or they feel claustrophobic.Positional therapy has a 35-40% higher adherence rate than CPAP. That’s huge. If you don’t use it, it doesn’t work. A device that you actually wear night after night is better than a machine you leave in the closet.
CPAP reduces overall AHI more than positional therapy. But for people with POSA, positional therapy can reduce supine AHI by 70-80%. That’s often enough to bring you from severe to mild-or even normal-apnea levels. Dr. David White, former president of the American Academy of Sleep Medicine, says for the right patient, positional therapy can be “remarkably effective.”
Who Should Try It
Not everyone with sleep apnea benefits from positional therapy. You need to have positional OSA. That means your apnea is much worse on your back. A sleep study must show your supine AHI is at least double your side AHI.Doctors usually recommend positional therapy for mild to moderate cases (AHI 5-30) where the position dependency is clear. If your AHI is above 30 and you have apnea no matter your position, CPAP or another treatment is likely needed.
It’s also not ideal for people with central sleep apnea, where the brain fails to signal the body to breathe. Positional therapy helps obstructive apnea-the kind caused by blocked airways-not central apnea. That said, side sleeping can still help reduce snoring and improve oxygen levels in central apnea patients, even if it doesn’t fix the root cause.
Getting Started
If you think you might have positional OSA, start with a sleep study that includes positional data. Many labs now track where you sleep and how many events happen in each position. Don’t assume your diagnosis is complete if it doesn’t break down AHI by position.Once you know you’re a candidate:
- Try the tennis ball technique for a week. It’s free. See if you can adapt.
- Use a body pillow or wedge pillow to help you stay on your side.
- Keep your head slightly elevated. A pillow that keeps your neck neutral helps keep your airway open.
- If you’re still rolling onto your back after two weeks, consider a device like NightBalance or SPT.
Most people need two weeks to adjust. The goal isn’t perfection-it’s reducing supine time to under 10%. Even cutting your back-sleeping time in half can cut your apnea events by half.
What the Market Offers
The market for positional therapy has grown fast. You can find:- DIY solutions: Tennis balls, $0. You can make this yourself.
- Positional pillows: $20-$50. Designed to keep you on your side.
- Wearable trainers: $300-$500. Devices like NightBalance, SPT, or Smart Nora.
Prices have dropped slightly since 2023, and insurance sometimes covers wearable devices if prescribed by a sleep doctor. Check with your provider. Some HSA/FSA accounts will reimburse you.
The Bigger Picture
Sleep apnea isn’t just about snoring. It’s linked to high blood pressure, heart disease, stroke, and diabetes. The supine position doesn’t just cause breathing pauses-it increases stress on your cardiovascular system. Studies suggest that reducing supine sleep may lower heart failure risk and reduce nighttime blood pressure spikes.But here’s the catch: most people never find out they have positional OSA. Their sleep study doesn’t break down the data by position. They’re told they have apnea, prescribed CPAP, and assume that’s the only option. They don’t realize a simple change in sleep position could eliminate their need for a machine.
Positional therapy isn’t a miracle cure. But for the right person, it’s one of the most effective, least invasive, and easiest-to-adhere-to treatments available. It doesn’t require surgery. It doesn’t need a mask. It just needs you to stop sleeping on your back.
Can sleeping on my side really fix sleep apnea?
Yes-for people with positional obstructive sleep apnea (POSA), side sleeping can dramatically reduce or even eliminate breathing pauses. Studies show that when patients avoid sleeping on their back, their apnea-hypopnea index (AHI) can drop by 70% or more. For many, this brings them from moderate to mild or normal apnea levels without any other treatment.
Is the tennis ball method effective?
It can be, but it’s not ideal for long-term use. The tennis ball technique works by making it uncomfortable to roll onto your back. About 45% of people stop using it within three months because it causes pain or disrupts sleep. It’s a good starting point to test if positional therapy helps, but most people switch to a wearable device like the Sleep Position Trainer for better comfort and adherence.
Do I need a sleep study to try positional therapy?
Yes, you should. Not everyone with sleep apnea has positional OSA. A sleep study that breaks down your apnea events by position is the only way to confirm if you’re a candidate. If your AHI isn’t at least twice as high on your back as on your side, positional therapy won’t help much. Don’t guess-get tested.
How does positional therapy compare to CPAP?
CPAP reduces overall apnea more than positional therapy, but people stick with positional therapy much longer. Adherence rates for CPAP are around 50-60%. For positional therapy, they’re 35-40% higher. If you can’t tolerate a mask or find CPAP too noisy, positional therapy can be a better long-term solution-if you have positional OSA.
Are positional therapy devices covered by insurance?
Sometimes. Devices like NightBalance or Sleep Position Trainer are often eligible for reimbursement through HSA or FSA accounts if prescribed by a sleep doctor. Some insurance plans cover them under durable medical equipment, especially if you’ve tried CPAP and failed. Always check with your provider and get a written recommendation from your sleep specialist.
Can I use positional therapy if I have central sleep apnea?
It’s less effective. Central sleep apnea is caused by the brain not signaling the body to breathe, not by airway blockage. Side sleeping may help reduce snoring and improve oxygen levels slightly, but it won’t fix the underlying issue. If you have central apnea, your doctor will likely recommend other treatments like adaptive servo-ventilation (ASV) or oxygen therapy.
How long does it take to see results from positional therapy?
Many people notice less snoring and better sleep within the first few nights. Objective improvements in breathing events usually show up after one to two weeks of consistent use. For best results, combine positional therapy with head elevation and avoid alcohol or sedatives before bed-they relax throat muscles and worsen apnea regardless of position.
Next Steps
If you’re tired of waking up gasping or your partner says you snore like a chainsaw, don’t just accept it as normal. Ask your doctor for a sleep study that includes positional data. If you have positional OSA, you’re not stuck with CPAP. You have a simpler, more comfortable option that works-and that more people stick with.Positional therapy isn’t magic. But it’s science. And for thousands of people, it’s the reason they finally sleep through the night.






evelyn wellding
January 16, 2026 AT 22:08Bianca Leonhardt
January 18, 2026 AT 16:31Travis Craw
January 20, 2026 AT 13:08vivek kumar
January 20, 2026 AT 18:38Riya Katyal
January 22, 2026 AT 05:41Henry Ip
January 23, 2026 AT 12:59swarnima singh
January 25, 2026 AT 12:52Isabella Reid
January 25, 2026 AT 14:15kanchan tiwari
January 26, 2026 AT 20:53Corey Chrisinger
January 28, 2026 AT 10:16Christina Bilotti
January 28, 2026 AT 18:02brooke wright
January 29, 2026 AT 20:08Nick Cole
January 31, 2026 AT 03:51Nicholas Gabriel
January 31, 2026 AT 15:33Cheryl Griffith
January 31, 2026 AT 16:19