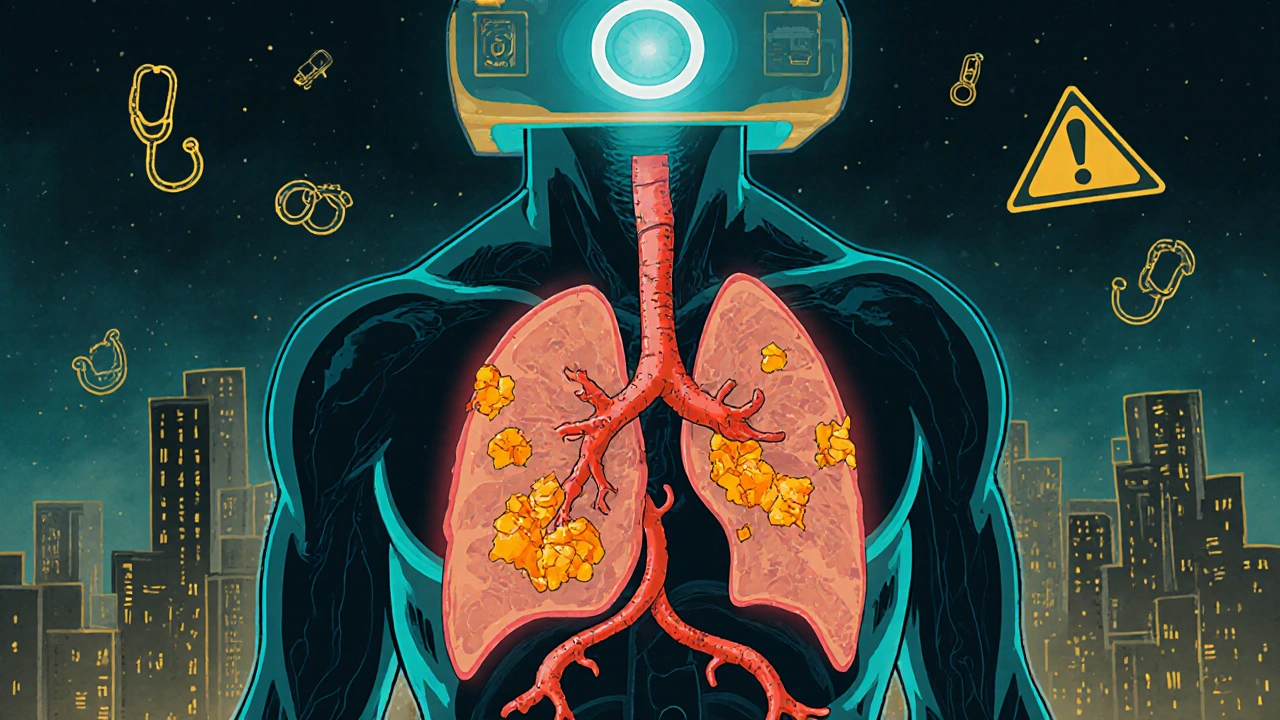
Most people don’t know their arteries are quietly clogging up years before they feel any chest pain or shortness of breath. That’s where a coronary calcium score comes in - a simple, non-invasive CT scan that shows exactly how much calcified plaque is building up in your heart’s arteries. It doesn’t require needles, dye, or fasting. You lie down, hold your breath for 10 seconds, and in under five minutes, you get a number that tells you more about your heart risk than most blood tests ever could.
What the Score Actually Measures
The coronary calcium score doesn’t measure blood flow or blockages. It measures calcium. And calcium doesn’t just appear out of nowhere - it’s a sign that plaque has been forming for years. When fatty deposits (plaque) build up inside your coronary arteries, your body tries to repair the damage by laying down calcium. That’s what the CT scan picks up. It’s like finding rust on a pipe - it doesn’t mean the pipe is fully clogged yet, but it tells you the problem started long ago.
This test uses a special type of CT scanner - either multidetector CT (MDCT) or electron beam CT - to take hundreds of images of your heart during a single breath-hold. The machine doesn’t need contrast dye, unlike other heart scans. Radiation exposure is low - about the same as a mammogram - between 1 and 3 mSv. The result? A single number called the Agatston Score, named after the radiologist who created it in 1990. It’s calculated by measuring the area and density of each calcium spot in your arteries.
What Your Score Means
A score of zero doesn’t guarantee you’re heart-healthy forever, but it does mean no calcified plaque has been detected yet. That’s the best-case scenario. Anything above zero? That’s evidence of coronary artery disease, even if you feel fine.
- 1-10: Minimal plaque. Low risk, but not zero. Time to pay attention to lifestyle.
- 11-100: Mild plaque. You have early disease. Your risk of a heart event is higher than most people your age.
- 101-400: Moderate plaque. This puts you in the 75% increased risk category for heart attack or stroke over the next 10 years.
- 401+: Extensive plaque. High risk. This level often means significant narrowing of arteries and calls for aggressive treatment.
Doctors don’t just look at the number alone. They compare it to others your age, sex, and ethnicity using the MESA Percentile. For example, a score of 150 might be normal for a 65-year-old man but very high for a 50-year-old woman. That’s why context matters.
Why It Beats Traditional Risk Calculators
Most doctors use tools like the Pooled Cohort Equations to estimate your heart risk based on age, cholesterol, blood pressure, and smoking status. But here’s the problem: those tools get it wrong about 20-30% of the time - especially for people in the so-called “intermediate risk” group.
That’s where the calcium score changes everything. Studies show it reclassifies risk in 40-50% of people who were previously labeled as “moderate risk.” Some are told they’re low risk - but their score is 300. Others are told they need statins - but their score is zero. In one study published in JAMA Internal Medicine, calcium scoring helped identify 35% of patients who should have been on statins but weren’t.
It’s not magic. It’s physics. The scan sees the actual damage in your arteries. Blood tests guess. This one shows.

What It Can’t Do
Here’s the catch: calcium scans only see calcified plaque. About 20-30% of plaque is soft - not yet hardened with calcium. That kind of plaque can still rupture and cause a heart attack, but it won’t show up on this scan. That’s why a normal score doesn’t mean you’re safe forever. If you have high cholesterol, smoke, or have diabetes, you still need to manage your risk.
For people with kidney disease, calcium can build up in arteries for reasons unrelated to heart disease. That can make the score misleadingly high. That’s why doctors don’t recommend this test for everyone - only those with intermediate risk and no symptoms.
Who Should Get Tested?
The American College of Cardiology and American Heart Association recommend this scan for adults aged 40-75 who are at intermediate risk - meaning a 7.5% to 20% chance of a heart event in the next 10 years. That includes people with:
- High LDL cholesterol (160 mg/dL or more)
- High blood pressure
- Smoking history
- Family history of early heart disease
- Diabetes
It’s not for people with symptoms like chest pain, shortness of breath, or known heart disease. Those patients need different tests. And it’s not for young, healthy people with no risk factors - their score will almost always be zero, and the test won’t add value.
What Happens After the Scan?
If your score is zero? Keep doing what you’re doing - eat well, move, don’t smoke. But keep checking in with your doctor.
If your score is above 100? That’s when things get serious. Most cardiologists will recommend:
- High-intensity statins if your score is above 300, regardless of other risk factors
- Medication to control blood pressure and cholesterol
- Lifestyle changes - diet, exercise, quitting smoking - as non-negotiable
One patient from Reddit, age 52, had a score of 142 - higher than 78% of men his age. He’d ignored his doctor’s advice to take statins for years. After seeing the number, he quit smoking and started medication. “It scared me into action,” he wrote. That’s the power of this test. It turns abstract risk into a concrete number you can’t ignore.

Insurance and Cost
Here’s the frustrating part: insurance doesn’t always cover it. Medicare doesn’t pay for it as part of the Annual Wellness Visit. Some private insurers will cover it if your doctor says it’s medically necessary - but others won’t. Out-of-pocket costs range from $100 to $300, depending on where you live and which facility you use.
A 2023 survey found that 41% of commercially insured patients had to pay part or all of the cost themselves. That’s a barrier for many, especially since the test can prevent expensive heart attacks down the line. In the U.S., about 2.1 million scans were done in 2022 - up 17% from the year before - but only 15% of eligible patients actually get tested.
The Future of Calcium Scoring
Technology is making it better. New AI algorithms can cut radiation exposure by 40% without losing image quality. Research is underway to define exact thresholds for when to start or increase medications based on the score. The NIH is funding a 10,000-person study to determine if using calcium scores to guide treatment can actually reduce heart attacks.
More cardiologists are pushing for wider use. In a 2023 survey, 87% said they’d recommend it more often if insurance coverage improved. The European Society of Cardiology now recommends it as a first-line test for people with a family history of early heart disease.
This isn’t just a test. It’s a turning point. For people who’ve been told they’re “fine” by traditional checks, it’s a wake-up call. For others, it’s confirmation that their lifestyle changes are working. And for doctors, it’s a tool to stop guessing and start treating with precision.
What to Do Next
If you’re between 40 and 75 and have even one risk factor - high cholesterol, smoking, high blood pressure, or a family history - talk to your doctor about a coronary calcium scan. Don’t wait for symptoms. Don’t assume your blood work is enough. Ask: “Could a calcium score help me understand my real risk?”
If you’ve already had the test and your score was above zero, don’t panic. Use it as a roadmap. Work with your doctor to lower your score over time. Statins, diet, exercise, and quitting smoking can slow or even reduce plaque buildup. The goal isn’t to erase the score - it’s to stop it from getting worse.
Heart disease doesn’t announce itself. But your arteries do. And now, with a simple scan, you can hear what they’re saying before it’s too late.
Is a coronary calcium scan the same as a heart CT angiogram?
No. A coronary calcium scan only looks for calcium in the arteries and doesn’t use contrast dye. A CT angiogram (CCTA) uses contrast dye to show both calcified and soft plaque, giving a detailed view of blockages. CCTA is more detailed but involves higher radiation (5-15 mSv) and is usually reserved for people with symptoms or abnormal stress tests.
Can a calcium score be too high?
There’s no upper limit that makes the test invalid. A score over 1,000 means extensive plaque and high risk - but it’s still useful. It tells your doctor you need aggressive treatment: high-intensity statins, blood pressure control, and lifestyle changes. The goal isn’t to avoid a high score - it’s to act on it.
Does a zero score mean I’m heart disease-free?
Not necessarily. A zero score means no calcified plaque was detected, but it doesn’t rule out soft, non-calcified plaque - which can still cause heart attacks. It also doesn’t protect you from future buildup. If you have risk factors like smoking or high cholesterol, you still need to manage them.
How often should I get a calcium scan?
If your score is zero and you have no risk factors, you may not need another for 5-10 years. If your score is above 100, repeat testing isn’t usually recommended unless your doctor suspects rapid progression. The focus after a high score is on treatment, not repeated scans.
Can I lower my calcium score?
You can’t remove calcium that’s already there - it’s like rust on a pipe. But you can stop it from growing. Studies show that statins, healthy diets, exercise, and quitting smoking can slow or even stabilize plaque buildup. In some cases, plaque volume can shrink over time, especially with aggressive treatment. The goal is to prevent rupture, not erase the score.





Katy Bell
November 21, 2025 AT 23:16This test is wild. I had mine done last year after my dad had a heart attack at 58. Score was 287. I thought I was fine because I ran 5Ks and ate salad. Turns out, I was just good at ignoring my body. Started statins. Quit soda. Now I sleep better. No regrets.
Ragini Sharma
November 22, 2025 AT 15:55so like… if i got a 0 score but still smoke 2 packs a day… am i just lying to myself? 😅
Suzan Wanjiru
November 24, 2025 AT 04:50Actually yeah you are. Soft plaque doesn’t show up. And smoking accelerates it like crazy. You’re basically playing Russian roulette with your coronary arteries and calling it a ‘clean bill of health’ because the machine didn’t see rust yet. Bad move.
Vivian C Martinez
November 25, 2025 AT 18:12That’s such a good point - a zero score is just a snapshot, not a guarantee. It’s like saying your car’s engine light is off, so you don’t need to change the oil. The damage is still happening underneath. The real win is using the score as motivation to fix the root causes, not just check a box.
Suresh Ramaiyan
November 26, 2025 AT 15:13I come from a family where heart disease hit everyone before 60. My dad had triple bypass at 54. I got my scan at 48 - score of 412. I was devastated. But then I started walking 8K steps daily, swapped rice for quinoa, and took my statin like clockwork. Two years later, my repeat scan? 398. It didn’t go down… but it didn’t climb either. That’s victory. Progress isn’t always about erasing the past. Sometimes it’s just about stopping it from getting worse.
Jennifer Shannon
November 27, 2025 AT 08:22Wow… I just cried reading that. I’m 51, I’ve been on statins for 7 years, and I still feel guilty every time I eat pizza. But seeing someone say ‘it didn’t go down, but it didn’t climb either’ - that’s the most comforting thing I’ve heard all week. I’ve been treating my score like a failure, but maybe… maybe it’s just a compass? Not a report card. Thank you for that.
Linda Rosie
November 27, 2025 AT 18:13Insurance should cover this. It’s cheaper than a heart attack.
Casper van Hoof
November 28, 2025 AT 08:02One must consider the epistemological implications of quantifying biological decay through radiological inference. The Agatston score, while empirically useful, is an ontological reduction - it collapses the complex, dynamic ecosystem of atherosclerosis into a singular, discrete integer. One might argue that this reification of pathology serves a utilitarian function in clinical practice, yet it risks fostering a false sense of epistemic certainty. The body is not a machine with discrete fault codes. It is a narrative written in lipids, inflammation, and time - and no algorithm can fully capture its poetry.
Bryson Carroll
November 30, 2025 AT 05:32Of course some guy in India with a 400 score is gonna feel good about his 398. That’s not progress that’s just not dying faster. Meanwhile I’m 42, no risk factors, zero score, and I still live like a human being. I eat butter, I don’t count steps, I drink wine. You people are scared of your own arteries. The real problem is that doctors sold you fear instead of facts.
Ross Ruprecht
December 1, 2025 AT 15:10bro i got my score done and it was 12. i didn’t even know what it meant so i just took a picture and posted it on instagram with a filter. got 300 likes. my mom cried. i think i’m fine.