Ulcerative Colitis: Causes, Symptoms, and Treatment Options
When your colon becomes chronically inflamed, it’s not just discomfort—it’s a daily battle. Ulcerative colitis, a type of inflammatory bowel disease that causes long-lasting inflammation and ulcers in the colon and rectum. Also known as UC, it’s not caused by stress or bad diet alone—it’s an autoimmune condition where your body attacks its own lining. Unlike Crohn’s disease, which can hit anywhere in the digestive tract, ulcerative colitis sticks to the innermost layer of the large intestine, starting at the rectum and moving upward. This matters because where it hits determines your symptoms, your treatment options, and how your life changes.
People with ulcerative colitis often deal with frequent diarrhea, bloody stools, abdominal cramps, and sudden urges to use the bathroom—sometimes so bad they can’t make it in time. Fatigue and weight loss aren’t just side effects; they’re signs your body is fighting a constant internal war. Flares come and go, sometimes triggered by infections, antibiotics, or even emotional stress. But here’s the thing: inflammatory bowel disease, a group of disorders including ulcerative colitis and Crohn’s disease that cause chronic gut inflammation isn’t one-size-fits-all. Two people with the same diagnosis can have totally different experiences. Some manage with diet and pills. Others need surgery. That’s why knowing your options is critical.
Bowel inflammation, the core problem in ulcerative colitis, happens when immune cells mistakenly target healthy tissue in the colon. This isn’t just irritation—it’s tissue damage that can lead to ulcers, scarring, and even increase cancer risk over time if left unchecked. That’s why monitoring isn’t optional. Regular colonoscopies, blood tests, and stool checks help catch changes early. Medications like aminosalicylates, corticosteroids, and biologics aim to calm the immune response. But they’re not magic bullets. Side effects happen. Some drugs work for months, others for years. And for a growing number of people, removing the colon becomes the most effective long-term solution.
What you’ll find below isn’t a list of generic advice. It’s a collection of real, practical comparisons and guides written by people who’ve lived through this. You’ll see how different treatments stack up against each other—what works, what doesn’t, and what side effects you might actually face. There are posts on steroid alternatives, how to handle flare-ups without relying on strong drugs, and even how lifestyle changes can reduce the frequency of attacks. You won’t find fluff. Just clear, no-nonsense info that helps you make smarter choices—whether you’re newly diagnosed, struggling with a flare, or thinking about surgery. This isn’t just about managing symptoms. It’s about taking back control.
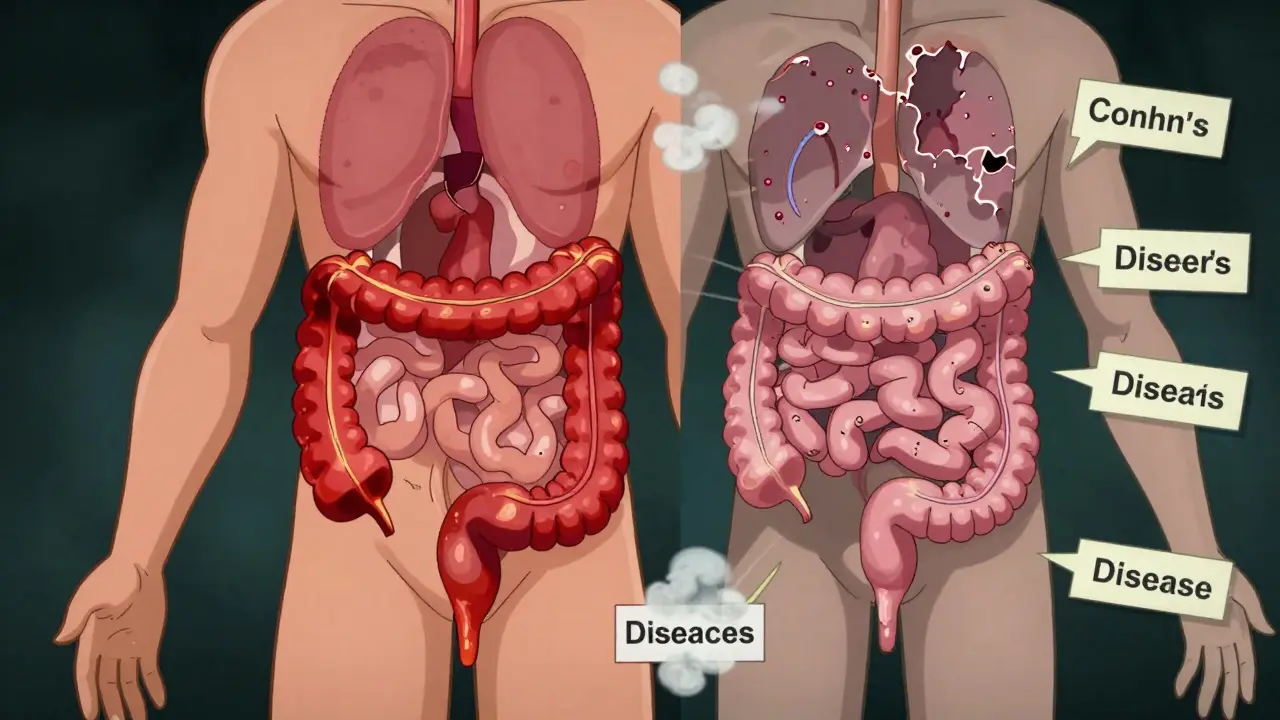
Inflammatory Bowel Disease: Crohn’s Disease vs. Ulcerative Colitis
Crohn’s disease and ulcerative colitis are two distinct forms of inflammatory bowel disease with different locations, depths of inflammation, complications, and treatments. Understanding the differences is key to managing symptoms and choosing the right care.

How Mesalamine Works in the Body to Treat Inflammatory Bowel Disease
Mesalamine is a targeted treatment for ulcerative colitis and mild Crohn's disease that reduces gut inflammation without suppressing the whole immune system. Learn how it works, its benefits, risks, and how it compares to other IBD medications.