Enzyme Deficiency: Causes, Symptoms, and Management
When talking about enzyme deficiency, a condition where the body lacks enough functional enzymes to carry out normal biochemical reactions. Also known as enzyme insufficiency, it can stem from genetic mutations, nutrient shortfalls, or acquired damage to organs that produce enzymes. Understanding this condition matters because enzymes act like tiny machines that keep metabolism humming; when they’re missing or broken, you can see everything from vague fatigue to serious organ failure.
One major genetic disorder, inherited mutations that impair enzyme production or function often lies at the heart of enzyme deficiency. For example, phenylketonuria (PKU) is a classic case where a faulty phenylalanine hydroxylase enzyme leads to toxic build‑up of phenylalanine, affecting brain development if not caught early. But not all deficiencies are inherited; a metabolic pathway, the series of enzyme‑driven steps that convert food into energy and building blocks can be disrupted by poor nutrition, liver disease, or exposure to certain drugs. When a pathway stalls, the body may accumulate harmful intermediates or starve for essential products, showing up as nausea, muscle weakness, or abnormal lab values. Diagnosing enzyme deficiency requires a clear step‑by‑step approach. First, clinicians look for clinical clues—unexplained growth delays, recurrent infections, or specific organ symptoms. Then they order targeted diagnostic testing, blood, urine, or genetic panels that measure enzyme activity or detect DNA mutations. In many cases, a simple newborn screen catches common deficiencies before symptoms appear, allowing early intervention. When a deficiency is confirmed, treatment options aim either to replace the missing enzyme, supply the downstream product, or block the harmful buildup. Enzyme replacement therapy (ERT) is a cornerstone for several inherited deficiencies such as Gaucher disease or Pompe disease. In ERT, lab‑manufactured enzymes are infused into the bloodstream, restoring the missing activity and halting disease progression. For non‑genetic cases, dietary adjustments—like supplementing vitamin B12 for methylmalonic acidemia—can effectively boost enzyme function. In some instances, organ transplantation (e.g., liver transplant for certain metabolic disorders) offers a permanent source of the needed enzyme.
Key Areas to Explore
Beyond diagnosis and therapy, it’s useful to know how lifestyle, monitoring, and emerging research fit into the picture. Regular follow‑up labs help track enzyme levels and catch any drift before complications arise. Patients often benefit from multidisciplinary care—dietitians, genetic counselors, and physiotherapists work together to manage symptoms and improve quality of life. On the research front, gene therapy is showing promise: delivering a correct copy of the enzyme gene straight into cells could one day replace lifelong enzyme replacement. All these pieces—genetic roots, metabolic impact, testing strategies, and treatment pathways—connect to give a full view of enzyme deficiency. Below you’ll find articles that break down specific conditions, compare treatment options, and offer practical tips for living with or managing these disorders. Dive in to see how each topic ties back to the core concepts we’ve just covered, and discover actionable insights you can apply right away.
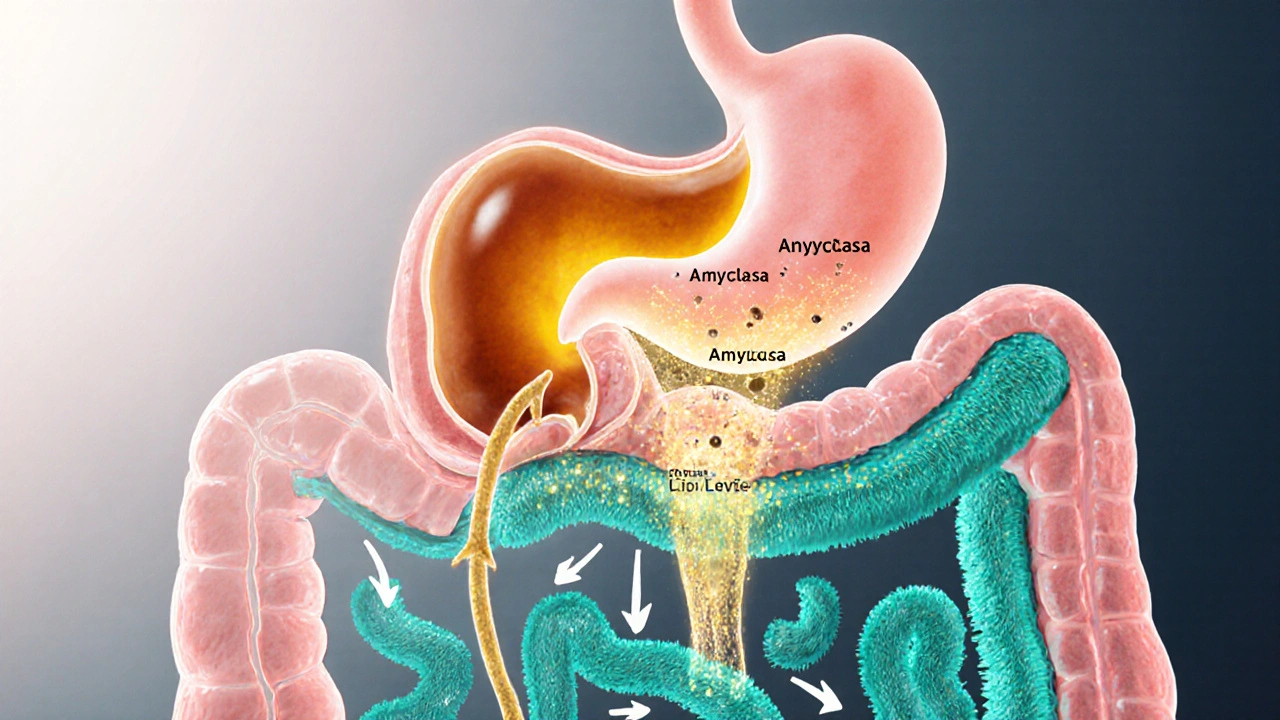
Why Digestive Enzymes Matter for Proper Food Absorption
Learn why digestive enzymes are vital for nutrient absorption, how deficiencies cause symptoms, and practical ways-through diet, lifestyle, or supplements-to keep your gut working efficiently.