Some medications work like a tightrope walk - one step too far, and things can go wrong fast. These are called narrow therapeutic index drugs, or NTI drugs. They’re not rare, but they’re dangerous if not handled with care. If you’re taking one, you need to understand how they work, why small changes matter, and what you can do to stay safe.
What Exactly Is a Narrow Therapeutic Index?
Every drug has a sweet spot - the amount that works without hurting you. For most medicines, that range is wide. You can miss a dose or take it a little late, and nothing major happens. But with NTI drugs, the line between helping and harming is razor-thin.
The FDA defines them as drugs where even tiny changes in your blood level - as little as 10% - can cause serious harm. Too little, and the drug doesn’t work. Too much, and it becomes toxic. Think of it like filling a glass with water: if the glass is huge, you can spill a little and still be fine. But if the glass is only big enough for one sip, a single drop overflows.
For example, warfarin (Coumadin) keeps blood from clotting. The right level means you’re protected from strokes. But if your blood level rises just a bit too high, you could bleed internally. Lithium helps stabilize mood in bipolar disorder, but levels above 1.5 mmol/L can cause confusion, tremors, or even seizures. There’s no room for guesswork.
Common NTI Drugs You Might Be Taking
You might not realize you’re on an NTI drug unless your doctor or pharmacist tells you. Here are the most common ones:
- Warfarin - Used to prevent clots. Requires regular INR blood tests.
- Lithium - Treats bipolar disorder. Needs blood level checks every few months.
- Levothyroxine - Replaces thyroid hormone. Even small switches in brand can throw off your levels.
- Digoxin - Helps heart rhythm. Toxicity can cause dangerous irregular beats.
- Tacrolimus - Used after organ transplants. Too low = rejection. Too high = kidney damage.
- Phenytoin and Carbamazepine - Anti-seizure drugs. Small changes can trigger seizures or toxicity.
- Methotrexate - Used for autoimmune diseases and some cancers. Overdose can damage bone marrow.
These aren’t “bad” drugs. They’re powerful, life-saving tools - but only when used precisely. That’s why they come with extra rules.
Why Generic Swaps Can Be Risky
Many patients get switched from brand-name to generic versions to save money. For most drugs, that’s fine. But for NTI drugs, it’s not always safe.
Generic drugs must be “bioequivalent” - meaning they work the same way as the brand. For most medicines, that means their blood levels can vary by up to 25% and still be considered acceptable. But for NTI drugs, that’s too much. A 25% drop could mean the drug stops working. A 25% rise could poison you.
That’s why the FDA and EMA require stricter standards for NTI generics. Instead of 80%-125% equivalence, they demand 90%-111%. That’s a much tighter range. Still, even within that range, differences in fillers, coatings, or how the pill breaks down in your gut can change how your body absorbs the drug.
Real stories prove this isn’t theoretical. One patient switched from brand Coumadin to a generic and saw their INR jump from 2.5 to 4.1 in just a week - a dangerous level that led to emergency treatment. Another person on levothyroxine noticed their TSH level went from 1.8 to 8.4 after switching generic brands - causing fatigue, weight gain, and depression. These aren’t rare cases. Surveys show over 60% of patients on NTI drugs have had to adjust their dose after a switch.
Monitoring Is Not Optional - It’s Lifesaving
If you’re on an NTI drug, regular blood tests aren’t a suggestion. They’re part of your treatment plan.
- Warfarin users typically get INR tests every 1 to 4 weeks, especially when starting or changing doses.
- Lithium levels are checked every 3 to 6 months, or more often if your dose changes or you get sick.
- Tacrolimus levels are checked twice a week right after a transplant, then less often as you stabilize.
- Levothyroxine patients usually get TSH tested every 6 to 8 weeks after a dose change.
These tests aren’t just paperwork. They’re your early warning system. Your doctor uses them to catch problems before you feel sick. Skipping a test might seem harmless - until you start bleeding, having seizures, or your transplanted organ starts failing.
Keep a log. Write down your test results, symptoms, and any changes in how you feel. Patients who track their own data have 32% fewer bad reactions. That’s not luck - it’s control.
What You Can Do to Stay Safe
You don’t need to be a scientist to manage an NTI drug. But you do need to be consistent and informed.
- Never switch brands without talking to your doctor. Even if the pharmacy says it’s “the same,” ask if it’s the same manufacturer. Some states, like North Carolina, require pharmacist approval before switching NTI generics.
- Stick to the same pharmacy. Different pharmacies may stock different generic versions. Staying at one place reduces the chance of an unexpected switch.
- Know your symptoms. Learn what under-dosing and over-dosing feel like. For warfarin: bruising easily or blood in urine = too high. New swelling or chest pain = too low. For lithium: shaky hands, confusion, nausea = too high. Feeling depressed or tired = too low.
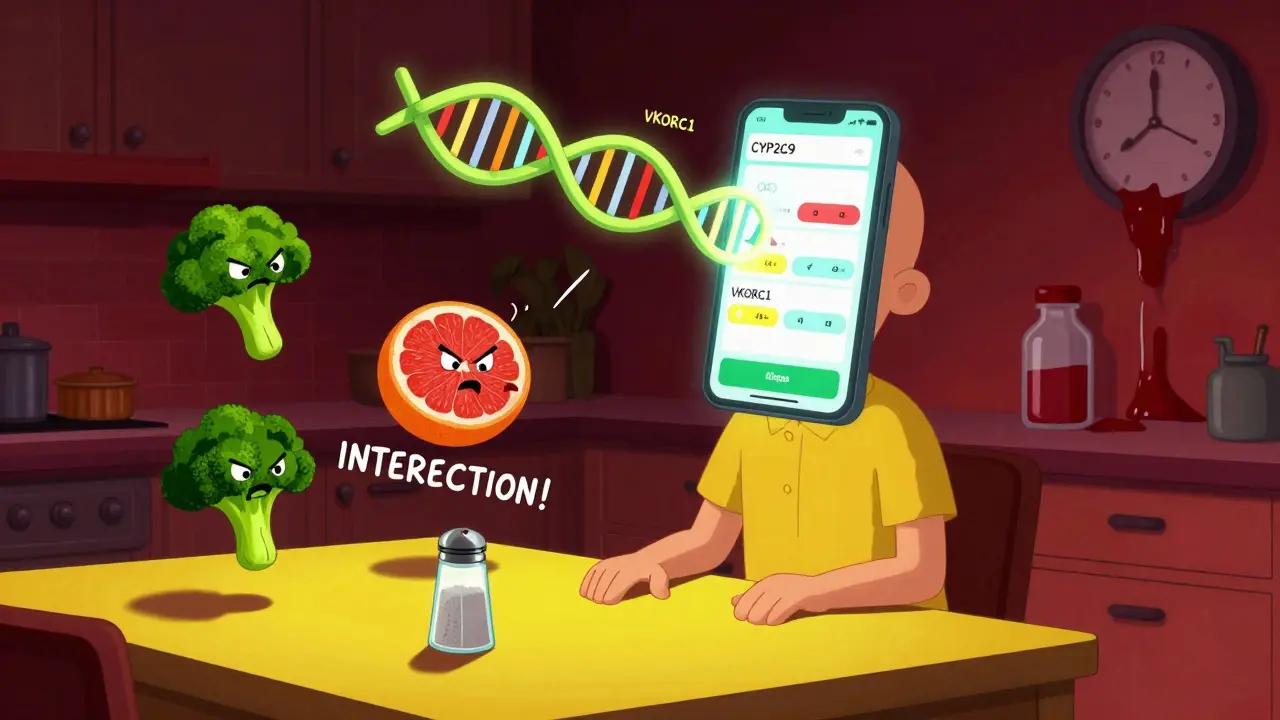
- Watch what you eat and drink. Vitamin K in leafy greens can weaken warfarin. Salt substitutes and dehydration can raise lithium levels. Grapefruit juice can interfere with tacrolimus and carbamazepine.
- Carry a list. Keep a printed or digital list of all your NTI drugs, your current dose, and your last test result. Emergency responders need this info fast.
The Future Is Personalized
Science is catching up. Researchers are learning that genetics play a big role in how your body handles NTI drugs. For example, your CYP2C9 and VKORC1 genes affect how you break down warfarin. Some people need half the dose of others just because of their DNA.
By 2026, genetic testing before starting certain NTI drugs may become standard. Early studies show this could cut adverse events by up to 35%. Apps are also helping - FDA-cleared tools now let you log doses, track symptoms, and sync lab results with your doctor.
But even with better tech, the core rule stays the same: precision matters. No shortcuts. No guessing. No skipping tests.
What Happens If You Ignore the Rules?
NTI drugs account for only 5-7% of all prescriptions, but they cause nearly 15% of serious drug-related hospitalizations. That’s because when they go wrong, they go wrong hard.
A patient on tacrolimus who gets a different generic might not feel sick at first - but their kidney function could start dropping. A person on levothyroxine might think their fatigue is just stress - but their TSH could be through the roof. These problems don’t always show up right away. That’s why monitoring is your best defense.
Don’t assume your doctor will catch everything. You’re the one who knows your body best. If you feel different - even a little - speak up. Ask for a blood test. Don’t wait.
Are all generic drugs unsafe for NTI medications?
No. Many generic versions of NTI drugs are safe and effective. But they must meet stricter bioequivalence standards (90%-111%) compared to regular drugs. The risk comes from switching between different generic brands without monitoring. Staying on the same manufacturer’s version reduces risk. Always check with your pharmacist or doctor before switching.
Can I stop taking my NTI drug if I feel fine?
Never stop or change your dose without talking to your doctor. Even if you feel fine, your blood levels might be outside the safe range. For example, someone on levothyroxine might feel okay but still have a TSH level that’s too high - which increases heart disease risk over time. NTI drugs work silently. Your symptoms don’t always tell the whole story.
Why do I need blood tests so often?
Because your body’s response to these drugs can change. Weight, diet, other medications, illness, or even stress can alter how your body absorbs or breaks down the drug. Blood tests are the only way to know if your level is still in the safe zone. Waiting until you feel sick means you’re already at risk.
What should I do if I miss a dose?
Don’t double up. Call your doctor or pharmacist for advice. For some NTI drugs like warfarin, missing a dose can increase clot risk. For others like lithium, skipping doses can cause mood swings or relapse. Each drug has different rules. Never guess - always ask.
Can I use over-the-counter supplements with my NTI drug?
Many supplements interact dangerously with NTI drugs. St. John’s wort can lower levels of tacrolimus and carbamazepine. Calcium and iron supplements can block levothyroxine. Even magnesium or fish oil can affect warfarin. Always tell your doctor about every supplement, herb, or vitamin you take - even if you think it’s harmless.
Final Thought: You’re the Key to Your Safety
NTI drugs are not a punishment. They’re a tool - one that requires your full attention. You don’t need to be perfect. But you do need to be consistent. Track your doses. Show up for your tests. Speak up when something feels off. Your life doesn’t depend on a miracle drug. It depends on your awareness.




amanda s
December 16, 2025 AT 15:50This is why I refuse to take generics-period. My cousin died because they switched her warfarin brand and no one told her. They call it ‘cost-saving’ but it’s just corporate greed wrapped in a white coat. I’m not a lab rat.
Raven C
December 18, 2025 AT 12:30One must, with the utmost gravity, acknowledge that the pharmacokinetic variability inherent in non-brand NTI agents constitutes a profound public health liability. The FDA’s 90–111% bioequivalence threshold is, frankly, an abdication of scientific rigor. One wonders whether the regulatory apparatus has been captured by pharmaceutical lobbying interests.
Jessica Salgado
December 19, 2025 AT 23:32I’ve been on levothyroxine for 12 years, and I swear by keeping the same pharmacy and writing down every TSH result in a little notebook. I even took a photo of my last lab slip and saved it in my phone. When I switched to a different generic last year? My fatigue came back like a ghost. I called my doctor the same day. Don’t ignore the small stuff-it’s the big stuff in disguise.
Chris Van Horn
December 21, 2025 AT 11:05Actually, the data on generic NTI drug variability is overstated. Most studies show no significant clinical difference when properly monitored. The real issue is patient noncompliance and poor doctor-patient communication-not the generics themselves. Also, ‘Coumadin’ is a brand name; the generic is warfarin. Stop being dramatic.
Steven Lavoie
December 22, 2025 AT 22:14As someone who’s had a kidney transplant, I can say this: tacrolimus saved my life. But I’ve been on the exact same generic brand since 2019. My levels are rock solid. The key? Consistency. Don’t switch unless your doctor says so-and even then, test before and after. I track everything. It’s not hard. It’s just necessary.
Michael Whitaker
December 24, 2025 AT 06:10It’s fascinating how people treat NTI drugs like they’re magic bullets. The truth? They’re just chemicals. Your body is the real variable. Genetics, gut flora, even your sleep schedule changes how they work. So yes, test often. But don’t fetishize the lab results. Your symptoms matter too. Balance, not fear.
Brooks Beveridge
December 25, 2025 AT 17:14You got this. Seriously. I know it feels overwhelming, but you’re not alone. Keep that log. Talk to your pharmacist. Ask questions. Even if you mess up once, just get back on track. That’s what matters. 💪🩺
Anu radha
December 26, 2025 AT 13:50I take lithium. My doctor checks my blood every 3 months. I feel okay, so I trust him. Thank you for this post. I feel less scared now.
Jigar shah
December 27, 2025 AT 20:14Interesting. I’m curious about the CYP2C9 polymorphism data in South Asian populations. Most studies are based on Caucasian cohorts. Has there been any research on how genetic variants like CYP2C9*3 affect warfarin dosing in Indian patients? Would be useful for personalized dosing here.
Sachin Bhorde
December 28, 2025 AT 22:10Yo, if you're on methotrexate or tacrolimus, DO NOT take turmeric or green tea extract. I'm a pharmacist, and I've seen too many people end up in the ER because they thought 'natural' = safe. Also, grapefruit? Big no. Your liver ain't gonna thank you. Stick to the script, folks. Your life's not a gamble.