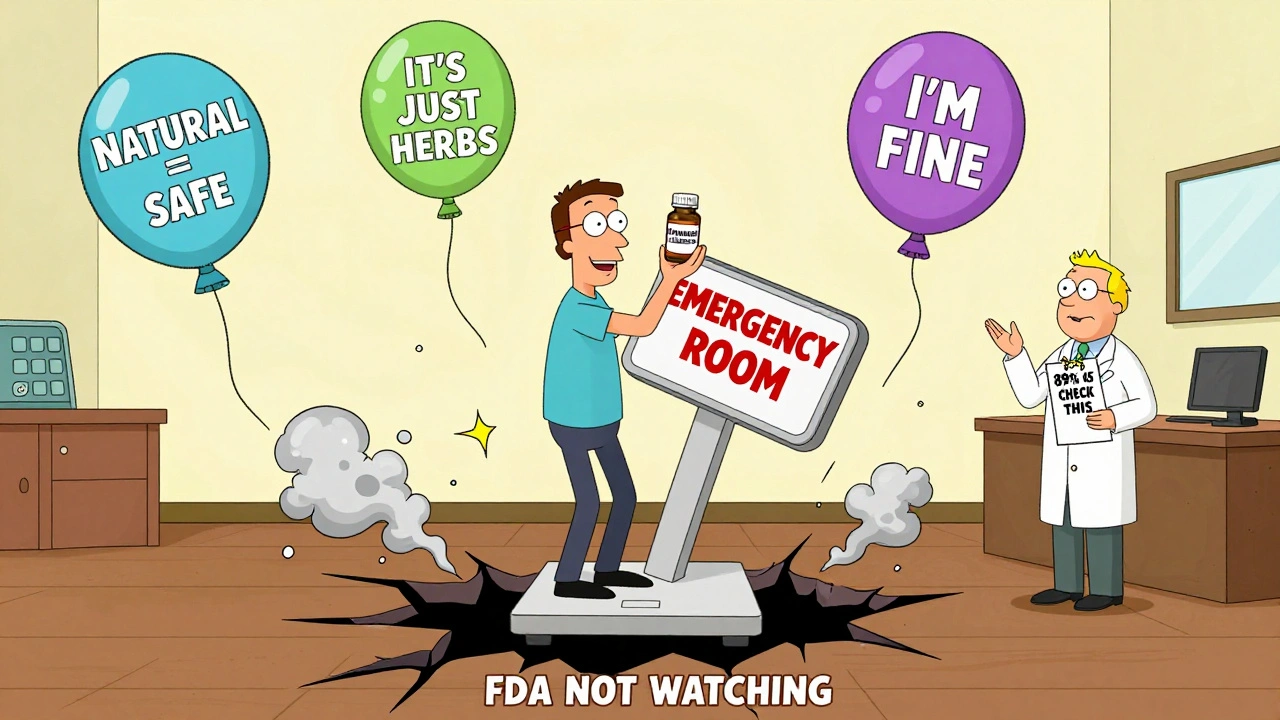
Every year, tens of thousands of people end up in emergency rooms because they took a supplement with their medicine - and didn’t realize it could be dangerous. You might think, It’s natural, so it’s safe. But that’s one of the most dangerous myths out there. St. John’s wort, for example, can drop your HIV medication levels by more than half. Ginkgo biloba can make your blood thinner than your warfarin dose intended. And if you’re on birth control, a daily supplement might be all it takes to get pregnant - without you knowing why.
Is this supplement going to mess with how my medicine works?
Your body doesn’t care if something is labeled “natural” or “herbal.” It only cares about what chemicals are in it and how they react with the drugs you’re already taking. The biggest culprits? Supplements that change how your liver processes medication. This happens through enzymes called cytochrome P450. St. John’s wort turns on CYP3A4 - a key enzyme that breaks down over 50% of all prescription drugs. That means your body clears out your medicine faster. Less medicine in your system = less effect. For someone on cyclosporine after a transplant, that’s a 50-60% drop in drug levels. That’s not a small risk. That’s organ rejection territory.
On the flip side, some supplements slow down how fast your body breaks down drugs. Vitamin E, especially at doses over 400 IU a day, can make warfarin stronger. That means your INR goes up. You’re at higher risk of bleeding - even from a minor cut. Ginkgo biloba does the same thing. In 15% of people taking both, INR levels jumped into dangerous zones. No warning. No label. Just a supplement on your nightstand.
Could this cause additive effects - like doubling down on side effects?
It’s not always about making a drug weaker or stronger. Sometimes, it’s about stacking effects. Take blood thinners and herbal supplements that also thin blood. Warfarin + ginkgo = higher bleeding risk. Aspirin + fish oil = same thing. Even turmeric, often praised for being anti-inflammatory, can increase bleeding risk when taken with anticoagulants. It’s not just about one supplement. It’s about the total load on your body.
Then there’s serotonin syndrome - a rare but deadly reaction. It happens when you combine supplements that boost serotonin with antidepressants. St. John’s wort is a big offender here. So is 5-HTP. And SAM-e. If you’re on an SSRI like fluoxetine (Prozac), adding one of these can push your serotonin levels too high. Symptoms? Confusion, rapid heartbeat, muscle stiffness, fever. People have ended up in the ICU because they thought “natural” meant harmless. It doesn’t.
Has this supplement been studied with my specific medication?
Here’s the hard truth: only about 15% of dietary supplements have any real research on interactions with prescription drugs. That means for most of what you’re taking - whether it’s ashwagandha, elderberry, or a “stress support” blend - there’s no data. No studies. No safety profile. Just guesswork.
St. John’s wort? Over 37 clinical trials. Ginkgo? Dozens. But what about that new “immune booster” you bought online? No studies. Not even close. And yet, you’re popping it every morning with your blood pressure pill. That’s not smart. That’s gambling with your health.
Even supplements that seem harmless can be risky. Milk thistle? Often used by people on liver-heavy meds like chemotherapy. Some studies suggest it might help reduce side effects - but only under strict medical supervision. Without that, you don’t know if it’s helping or interfering. And if your oncologist hasn’t reviewed it? You’re flying blind.

What symptoms should I watch for if something’s going wrong?
You need to know the red flags. Don’t wait for a hospital visit. Learn what to look for.
- For blood thinners: Unusual bruising, nosebleeds, blood in urine or stool, dizziness, headaches that won’t go away.
- For immunosuppressants: Fever, chills, sore throat, fatigue - signs your body can’t fight off infection because the drug isn’t working.
- For HIV meds: Sudden increase in viral load, unexplained weight loss, night sweats.
- For birth control: Breakthrough bleeding, missed periods, or - worst case - pregnancy.
- For serotonin syndrome: Agitation, confusion, rapid heart rate, muscle rigidity, high body temperature.
If you notice any of these after starting a supplement - stop it immediately. Call your doctor. Don’t wait. Don’t Google it. Don’t assume it’s “just a side effect.”
Are there safer alternatives to this supplement?
Not all supplements are created equal. Even within the same category, some have far fewer interactions. For example:
- Asian ginseng? High risk. Can raise blood pressure and interfere with blood thinners.
- American ginseng? Much lower risk. Better choice if you need energy support.
- St. John’s wort? Avoid completely if you’re on any prescription med.
- Milk thistle? Lower risk, but still needs monitoring if you’re on liver-metabolized drugs.
- Black cohosh? Generally low risk, but avoid if you have hormone-sensitive conditions.
Even something as simple as vitamin D can be tricky. High doses (over 4,000 IU/day) can raise calcium levels - which can interfere with heart meds like digoxin. So yes, even “safe” vitamins need context.
Ask your pharmacist: “Is there a version of this supplement that’s been tested and shown to be safer with my meds?” They’ve seen it all. They know the alternatives.
Who should I talk to before taking this?
Most people assume their doctor knows what they’re taking. They don’t. In a typical 15-minute appointment, doctors spend just 1.2 minutes asking about supplements. That’s not enough. And many patients don’t even mention them - because they don’t think it matters.
You need to be proactive. Bring a list. Include every pill, capsule, powder, and tincture. Even the ones you only take “once in a while.” Write down the brand and dose. Don’t say “I take ashwagandha.” Say “I take 600 mg of KSM-66 Ashwagandha daily.” Specifics matter.
Pharmacists are your best ally here. They’re trained to catch interactions. And since 2023, 89% of pharmacists in the U.S. now routinely screen for supplement-drug interactions during medication reviews. If you’re getting your prescriptions filled at a chain pharmacy, ask for a Medication Therapy Management session. It’s free. It’s confidential. And it could save your life.
What’s the real risk here?
Some companies say supplement interactions are “exceedingly rare.” That’s misleading. The CDC reports 23,000 emergency room visits a year because of supplement-drug interactions. One in five of those cases are serious - including strokes, organ failure, and death. And that’s just what gets reported. The real number? Likely much higher.
Why? Because most people never connect the dots. They take a supplement. They feel off. They blame stress. Or aging. Or bad sleep. They don’t think to look at what they added to their routine. And by the time they do, it’s too late.
The supplement industry is worth over $52 billion in the U.S. alone. But less than 3% of products have verified interaction data. The FDA doesn’t require pre-market safety testing. Labels are often wrong. Ingredients can be mislabeled by 70% in some cases. You’re not buying a product. You’re buying a gamble.
So ask yourself: Is this supplement worth the risk? If your medicine keeps you alive, or keeps your condition stable - then the answer is no. Not unless you’ve talked to a professional who knows your full health picture.
What’s changing - and what you need to know now
The good news? Things are starting to shift. As of January 2024, major electronic health record systems like Epic now require doctors to document supplement use. That means your list will actually be in your file. No more forgetting.
The FDA also launched the Dietary Supplement Ingredient Database (DSID-6) in 2023. It’s the first time they’re verifying actual ingredient amounts in supplements. That’s huge. It means someday, you might be able to check if your bottle actually contains what it says.
But right now? You can’t wait for regulation. You have to protect yourself. The system isn’t designed to keep you safe. You are.






Gwyneth Agnes
December 7, 2025 AT 23:21Stop taking supplements. Just stop. Your body doesn't need them.
Ashish Vazirani
December 8, 2025 AT 00:15Ohhh, so now we're blaming supplements? In India, we've been taking turmeric with everything for centuries-no ER visits, no drama. This is Western paranoia dressed up as science. Who funded this article? Pharma? Of course they are. They want you dependent on pills, not plants!
Mansi Bansal
December 9, 2025 AT 09:20While I appreciate the clinical rigor of this exposition, I must respectfully posit that the underlying epistemological framework is predicated upon a reductionist biomedical paradigm that overlooks the holistic ontologies of traditional healing systems. The conflation of pharmacokinetic interactions with moral hazard is not merely reductive-it is ethically fraught. One cannot equate the Ayurvedic use of ashwagandha with the commodified, unregulated American supplement industry. The cultural context is not incidental-it is constitutive.
Kay Jolie
December 9, 2025 AT 11:38Okay but have you considered the bioavailability profiles of standardized extracts versus raw herb powders? Like, if you’re taking a 600mg KSM-66 ashwagandha capsule, that’s a highly bioavailable, patented root extract with documented CYP3A4 modulation-whereas your ‘organic turmeric powder’ from the bazaar? Probably 3% curcuminoids, zero clinical data, and possibly laced with lead. The real issue isn’t supplements-it’s the lack of standardization and transparency. We need third-party verified labels, like NSF or USP. Until then, it’s just snake oil with a wellness influencer’s face on it.
pallavi khushwani
December 11, 2025 AT 08:36It’s wild how we treat food like medicine and medicine like food. We eat turmeric like it’s a spice, but take St. John’s wort like it’s a pill-same plant, different mindset. Maybe the problem isn’t the supplement. Maybe it’s the idea that we can just add something to fix a system we’re already breaking with stress, sleeplessness, and processed food. What if the real interaction is between our lifestyle and our fear of being unwell?
Dan Cole
December 11, 2025 AT 16:25You're all missing the fundamental point: the FDA doesn't regulate supplements because they're not drugs. That's not a loophole-it's a legal definition. And if you're dumb enough to assume 'natural' means 'safe,' you deserve the ER visit. This isn't about conspiracy. It's about basic biology. Enzymes don't care if you call it 'herbal harmony.' They metabolize chemicals. Period. If you can't grasp cytochrome P450, don't take supplements. Simple. No apologies.
Billy Schimmel
December 13, 2025 AT 12:15So... you’re telling me the guy who takes fish oil because his wife said it’s ‘good for the heart’ might accidentally bleed out because he’s on warfarin? Yeah. That’s the story of my uncle Bob. He died in 2018. Took ginkgo. Didn’t tell his doctor. Thought it was ‘just a brain booster.’ Rest in peace, Bob. You were the best. And also… kinda clueless.
Max Manoles
December 13, 2025 AT 22:06There’s a quiet epidemic here: people think their doctor knows what they’re taking. But doctors are overworked, underpaid, and asked to memorize 12,000 drug interactions while juggling 30 patients a day. The real failure isn’t the supplement-it’s the healthcare system that doesn’t make space for the truth. Bring a list. Write it down. Say it out loud. Even if it feels awkward. Your life isn’t a footnote.
Clare Fox
December 14, 2025 AT 09:05i used to take st. john’s wort for anxiety. then i got on a new antidep. and i just… felt weird. like my brain was on mute. didn’t connect it until i read this. stopped it. felt normal again. why do we think our bodies are these magic boxes that just ‘handle’ stuff? we’re not robots. we’re messy, chemical, fragile. and that’s okay. but we gotta pay attention.
Akash Takyar
December 14, 2025 AT 11:33Dear Readers, I commend the author for this timely and meticulously researched exposition. In the Indian context, where polypharmacy is common and self-medication is culturally entrenched, such awareness is not merely beneficial-it is imperative. I urge every individual to consult a registered pharmacist before initiating any herbal regimen. Remember: Knowledge is the most potent medicine. Let us not gamble with our vitality. Thank you.
Arjun Deva
December 14, 2025 AT 22:56Wait… so this whole thing is a distraction? The real danger is the pharmaceutical-industrial complex. They don’t want you healing naturally. They want you on pills forever. The CDC numbers? Fabricated. The FDA? Bought. The supplement industry? The only honest one left. You think your blood thinner is safe? Bet you don’t know what’s in that pill. Glyphosate. Microplastics. GMO fillers. They’re poisoning you slowly-and now they’re blaming turmeric. Classic.
Ibrahim Yakubu
December 15, 2025 AT 18:55Look, I’m a pharmacist in Lagos. I’ve seen people take artemisinin with malaria meds because they thought ‘more is better.’ I’ve seen people on HIV meds take bitter leaf tea and crash their viral load. This isn’t just American drama. It’s global. If you’re taking anything with your prescription-write it down. Show me. I don’t care if it’s ‘traditional.’ I care if you’re alive tomorrow. Period.