Drug Dechallenge Time Calculator
How It Works
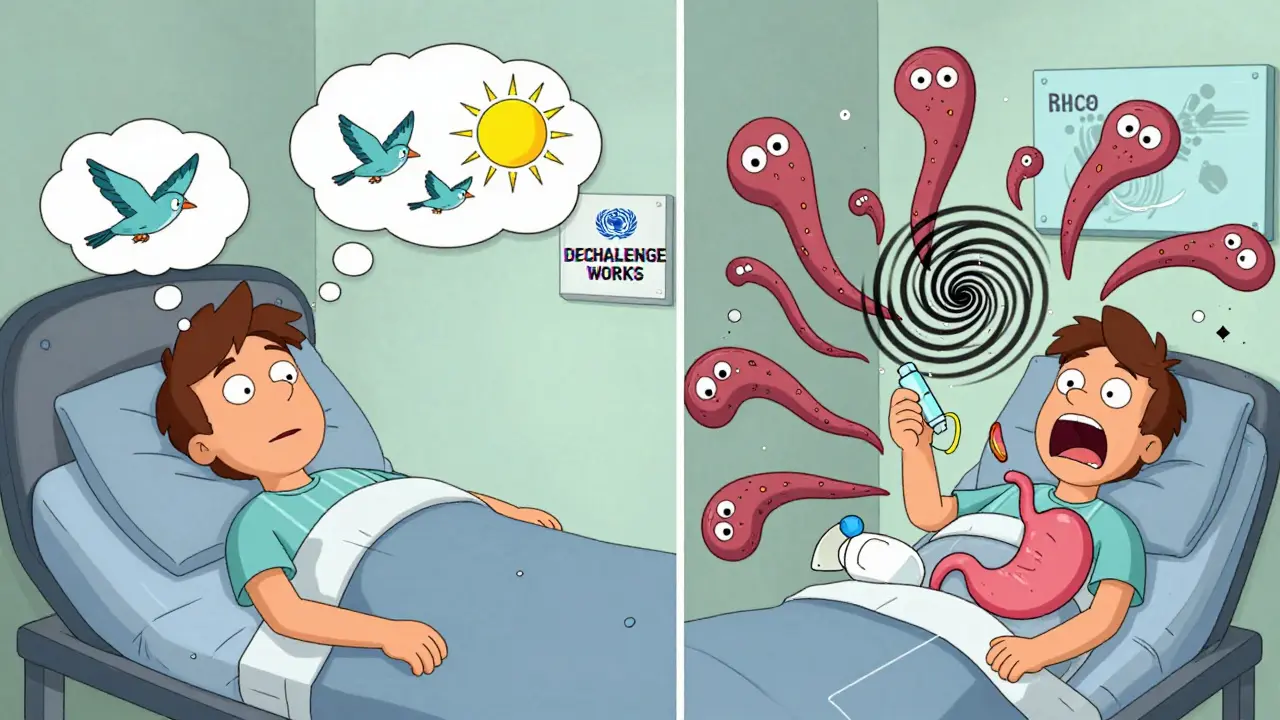
Dechallenge is stopping a suspected drug to see if symptoms improve. This calculator helps determine how long it might take for symptoms to resolve based on the drug's half-life and when symptoms appeared.
It typically takes 4-5 half-lives for a drug to be mostly eliminated from the body. Symptoms often improve after the drug is cleared, but sometimes take longer due to residual effects or other factors.
Have you ever been told to stop a medication because you developed a rash, dizziness, or nausea-and then felt better right away? That’s not just coincidence. It’s likely a dechallenge at work. And if your doctor later asked you to take the same drug again, just to see if the problem came back? That’s a rechallenge. These aren’t fancy medical jargon-they’re real, practical tools doctors use to figure out which drug is actually causing trouble.
Most people assume if a side effect shows up after taking a pill, the pill must be to blame. But that’s not always true. Sometimes symptoms appear around the same time as a new medication, but they’re caused by something else: stress, an infection, another drug, or even the underlying illness you’re being treated for. So how do you know for sure? That’s where dechallenge and rechallenge come in.
What Is Dechallenge?
Dechallenge means stopping the suspected drug and watching what happens. If your symptoms get better-or disappear-after you stop taking it, that’s called a positive dechallenge. It’s one of the strongest clues that the drug was causing the problem.
For example, someone develops a severe skin rash after starting a new antibiotic. The doctor tells them to stop the drug. Within five days, the rash fades. The redness goes down. The itching stops. That’s a clear positive dechallenge. It doesn’t prove 100% that the antibiotic caused it, but it makes it highly likely.
But not all dechallenges are clear-cut. Sometimes symptoms don’t fully go away-even after stopping the drug. That’s a negative dechallenge. It could mean the drug wasn’t the cause. Or it could mean the damage is permanent, like some types of nerve injury or liver scarring. In those cases, stopping the drug helps prevent further harm, but the original effect may linger.
Timing matters. If the side effect disappeared in two days after stopping a drug with a half-life of 12 hours, that makes sense. But if it took three weeks? That’s less likely to be connected. Doctors look at how long the drug stays in your body and whether the improvement matches that timeline.
What Is Rechallenge?
Rechallenge is when you take the drug again-on purpose-to see if the side effect returns. If it does, that’s powerful evidence. In fact, it’s the gold standard for proving a drug caused a reaction.
A classic case: a patient gets a fixed drug eruption-a dark, circular rash that always shows up in the same spot-after taking metronidazole. After stopping the drug, the rash fades over two weeks. Then, months later, the doctor gives them a tiny, controlled dose of metronidazole under supervision. Within 48 hours, the exact same rash reappears in the same spot. That’s a positive rechallenge. It’s not just correlation anymore. It’s cause and effect confirmed.
Rechallenge isn’t done lightly. If the side effect was life-threatening-like Stevens-Johnson Syndrome, toxic epidermal necrolysis, or drug-induced liver failure-rechallenge is almost never done. The risk is too high. Even for less severe reactions, it’s only done under strict medical supervision, with emergency equipment ready, and only after the patient gives full informed consent.
According to studies, when a rechallenge is successfully performed and the reaction returns, it confirms drug causality in 97% of cases under WHO-UMC guidelines. That’s stronger than any algorithm, lab test, or statistical model.
Why These Tests Matter More Than You Think
Imagine you’re a pharmacist reviewing a report that says, “Patient had dizziness after starting lisinopril.” Without dechallenge or rechallenge, that’s just a guess. But if the patient stopped lisinopril and the dizziness vanished-and then returned when they restarted it-that’s solid proof. That changes everything.
It means the patient can avoid that drug forever. It means their doctor won’t prescribe it to someone else with similar symptoms. It means drug safety databases get updated with real-world evidence, not just assumptions.
Without dechallenge and rechallenge, we’d be guessing a lot more. And in medicine, guessing can lead to harm. One wrong drug kept in a patient’s regimen could lead to kidney damage, heart rhythm problems, or even death.
These tests also help separate true drug reactions from placebo effects or coincidental events. If someone feels better after stopping a pill, but the improvement was just because they were feeling less stressed or got more sleep, the symptoms won’t come back with rechallenge. That’s how you tell the difference.

When Rechallenge Isn’t an Option
Let’s be clear: rechallenge is rare. In fact, fewer than 0.3% of serious adverse drug reaction investigations include it. Why? Because the risk can outweigh the benefit.
For example, if someone had a severe allergic reaction to penicillin that caused swelling of the throat and trouble breathing, no doctor would ever give them penicillin again-on purpose. The risk of death is too high. In those cases, doctors rely on dechallenge alone, plus skin testing or blood tests for specific antibodies.
Even for less dangerous reactions, ethical review boards and regulatory agencies require strict approval before rechallenge can happen. The FDA and European Medicines Agency both require documented informed consent, a clear medical rationale, and emergency protocols in place.
That’s why dechallenge is the workhorse of causality assessment. It’s used in about 85% of dermatological adverse reactions and 79% of liver injury cases. It’s safe, practical, and gives useful answers without putting the patient at risk.
How Doctors Use This in Real Life
In clinics, dechallenge and rechallenge aren’t always formal procedures. Often, they’re just smart clinical reasoning.
A patient on five different medications develops fatigue and nausea. The doctor doesn’t stop all five at once-that would make it impossible to know which one was the culprit. Instead, they stop one at a time, starting with the newest or most likely offender. They monitor symptoms for 7-14 days. If the fatigue lifts after stopping Drug A, but returns when Drug A is restarted (under supervision), that’s a clear signal.
Electronic health records now have built-in prompts that ask clinicians: “Was the drug discontinued? Did symptoms improve? Was it rechallenged?” This helps standardize reporting and makes data more useful for drug safety teams.
Pharmaceutical companies also rely on this data. When they submit safety reports to regulators, they’re required to include dechallenge outcomes. In 2023, 82% of major drug manufacturers required this data in post-marketing studies, according to PhRMA.
The New Tech Helping Dechallenge Get Better
Technology is making dechallenge more accurate. Wearable sensors can now track heart rate, skin temperature, and even subtle changes in movement or sleep patterns when a drug is stopped. In one 2023 study, sensors picked up objective signs of improvement in 78% of cases-compared to only 52% when relying on patient self-reports.
Researchers are also developing blood tests that can predict if someone is likely to have a reaction to a drug-without ever giving it to them. These tests look at genetic markers or immune cell behavior. One NIH study from April 2024 showed an 89% accuracy rate in predicting certain skin reactions.
But here’s the catch: even the best tech can’t replace the real-world test of stopping the drug and seeing what happens. As Dr. Elena Rodriguez from the WHO said in 2024, “No algorithm can substitute for the clinical reality of symptom resolution after drug discontinuation.”
What You Can Do
If you’re on a new medication and start feeling off, don’t just assume it’s “normal.” Write down your symptoms, when they started, and how bad they are. Tell your doctor. Ask: “Could this be from the new drug? What happens if I stop it?”
If your doctor suggests stopping a drug to see if symptoms improve, follow through-even if you feel better after a few days. That information helps them make better decisions for you and others.
And if you’ve ever had a reaction to a drug, make sure it’s documented in your medical record. Say: “I had a rash when I took X drug. Don’t give it to me again.” That simple step can prevent serious harm in the future.
Dechallenge and rechallenge aren’t just for doctors and researchers. They’re tools that belong to patients too. Understanding them helps you take control of your health-and keep dangerous drugs out of your treatment plan.
What’s the difference between dechallenge and rechallenge?
Dechallenge is stopping a drug to see if side effects go away. If they do, it suggests the drug caused them. Rechallenge is giving the drug back after symptoms have cleared-if the side effect returns, it confirms the drug is the cause. Dechallenge is common and safe; rechallenge is rare and only done under strict supervision.
Is rechallenge dangerous?
Yes, it can be. Rechallenge is risky because you’re intentionally exposing someone to a drug that previously caused harm. For severe reactions like anaphylaxis, liver failure, or life-threatening skin conditions, rechallenge is almost never done. It’s only considered for mild to moderate reactions, with full consent, medical supervision, and emergency plans in place.
Why not just use blood tests or genetic tests instead?
Blood and genetic tests can help predict reactions in some cases-like with certain antibiotics or seizure meds-but they don’t work for most side effects. Many reactions, like rashes, dizziness, or nausea, aren’t tied to a single gene or biomarker. Only dechallenge shows what actually happens in the real body, not just in a lab.
Can I do a dechallenge on my own by stopping a drug?
No. Stopping a drug without medical advice can be dangerous. Some medications need to be tapered off slowly, or stopping suddenly can cause withdrawal, rebound symptoms, or worsening of your original condition. Always talk to your doctor before stopping any prescribed drug.
How often do doctors use dechallenge and rechallenge?
Dechallenge is used in about 85% of skin-related drug reactions and 79% of liver injury cases. Rechallenge is used in less than 1% of cases overall because of safety concerns. In dermatology and allergy clinics, these tools are standard. In psychiatry or chronic disease care, they’re used less often because stopping medication can be risky for the patient’s stability.
Are these methods required by regulators?
Yes. Both the U.S. FDA and the European Medicines Agency require dechallenge information in safety reports for new and existing drugs. The WHO-UMC and CIOMS guidelines also list dechallenge and rechallenge as key criteria for determining if a drug caused an adverse reaction. Pharmaceutical companies must include this data in their global safety submissions.
Final Thought
Medicines save lives-but they can also hurt. Dechallenge and rechallenge are simple, low-tech, high-impact tools that turn suspicion into certainty. They don’t need fancy machines or expensive labs. Just careful observation, good communication, and a willingness to listen-to the patient, to the body, and to the evidence.
Next time you hear a doctor say, “Let’s stop this drug and see what happens,” know that they’re not guessing. They’re using one of the oldest, most reliable methods in medicine to keep you safe.







Katie Taylor
December 23, 2025 AT 12:35This is the kind of info every patient needs to know. I had a rash from amoxicillin and my doctor just told me to stop it-no explanation. Now I get it. Dechallenge saved me from years of misdiagnosis. Thank you for breaking this down.
Stop guessing. Start testing. Your body isn’t a lottery ticket.
Usha Sundar
December 24, 2025 AT 07:20Rechallenge? No thanks. I’m not volunteering to die for science.
Wilton Holliday
December 25, 2025 AT 05:34Love this breakdown! 🙌 Seriously, most people don’t realize how much of medicine is still guesswork. Dechallenge is like the OG diagnostic tool-no lab coat needed, just patience and observation.
And yes, doctors should ask: ‘Did you stop the med?’ before jumping to ‘new condition.’ Too many patients get mislabeled because no one checked the basics.
Keep sharing this stuff. It saves lives.
Pankaj Chaudhary IPS
December 27, 2025 AT 02:36In India, we often face the opposite problem: doctors prescribe multiple drugs at once and never dechallenge. Patients suffer for months because no one takes responsibility. This article should be mandatory reading for every medical student in South Asia.
Respect for the science. Respect for the patient. Dechallenge is not optional-it is ethical.
Aurora Daisy
December 27, 2025 AT 05:54Oh wow, so now we’re romanticizing stopping pills like it’s a spa day? Next you’ll tell me ‘rest and ice’ is a clinical trial.
97% accuracy? That’s not science. That’s hoping your patient doesn’t die before the rash fades.
Paula Villete
December 27, 2025 AT 20:41So let me get this straight: the gold standard for proving drug causality is… giving the patient the thing that almost killed them again? And we call this medicine?
Also, typo: ‘dechallenge’ is not a verb. But I’ll let it slide because this is actually useful. Mostly.
Still. Rechallenge sounds like a horror movie sequel. Don’t watch it. Don’t do it. Just… don’t.
Georgia Brach
December 29, 2025 AT 09:2585% usage rate? That’s not evidence-it’s confirmation bias. You’re assuming the drug is guilty because it was taken recently. Correlation isn’t causation, and neither is timing.
And where’s the control group? Where’s the double-blind? Where’s the peer review?
Real science doesn’t rely on ‘let’s stop it and see.’ That’s anecdote dressed in a white coat.
Isaac Bonillo Alcaina
December 30, 2025 AT 16:42Oh wow. Another article telling patients to stop their meds like they’re toddlers throwing tantrums. You think your ‘rash’ is from the pill? Maybe it’s from the stress of believing everything’s a pill’s fault.
Most side effects are placebo. Most ‘improvements’ after stopping are just regression to the mean.
Stop empowering people to self-diagnose. It’s dangerous. And stupid.
Joe Jeter
December 31, 2025 AT 20:07Rechallenge is a joke. If you had a bad reaction, you don’t get a second chance. You get a lifetime ban.
And if your doctor wants to rechallenge you? Run. Not walk. Run.
Also, why are we still using 1950s methods in 2024? We have AI, genomic mapping, and wearable biosensors-but nope, we’re still playing ‘guess which pill made you itchy.’
Sidra Khan
January 2, 2026 AT 12:34Dechallenge = stop the drug
Rechallenge = try to kill yourself again for science 😅
Also, I had a rash from ibuprofen. Stopped it. Gone. Rechallenged? Nope. I’m not a lab rat. I’m a human with a life to live.
Lu Jelonek
January 3, 2026 AT 16:02For those wondering why this matters: imagine being prescribed a drug you’re allergic to because your record says ‘possible reaction’ instead of ‘confirmed.’
Dechallenge turns ‘possible’ into ‘confirmed.’ That’s not just useful-it’s life-saving.
Always document your reactions. Even if it’s ‘just a rash.’ It’s not just ‘just’ anything. It’s data.
Ademola Madehin
January 5, 2026 AT 05:47Bro, I took that one antibiotic and my whole body turned into a fire alarm. Doctor said ‘stop it.’ I did. 2 days later? I was back to normal.
Then he gave me another one. Same thing. Now I just say ‘NO’ to anything that sounds like it’s from a sci-fi movie.
Dechallenge? Yeah, I did that. Without the doctor. Just me and my itching skin.
suhani mathur
January 5, 2026 AT 16:35Rechallenge is like asking your ex to come back… just to see if they’ll hurt you again.
Some lessons aren’t worth repeating.
Also, in India, we don’t even get dechallenge. Doctors just switch the drug and say ‘maybe this one works.’ No follow-up. No curiosity. Just… next.
Adarsh Dubey
January 6, 2026 AT 03:52Interesting read. I’ve seen both sides. My mom had liver enzyme spikes on a statin. Stopped it-levels normalized. Rechallenge? Never happened. Too risky.
But the fact that it resolved after stopping? That’s enough for us. We don’t need to prove it with danger to know what to avoid.
Dechallenge is the quiet hero of pharmacovigilance.
Bartholomew Henry Allen
January 7, 2026 AT 01:10Dechallenge and rechallenge are not medical procedures they are patient management strategies with no regulatory foundation and no standardized protocol
Pharmaceutical companies do not require this data and the FDA does not mandate it for approval
This article is misleading and dangerous