Opioid Overdose Prevention: Practical Tips, Tools, and Resources
When talking about opioid overdose prevention, the set of actions aimed at stopping fatal opioid intoxication before it happens. Also known as opioid safety, it blends education, medication management, and rapid‑response measures to keep communities safe.
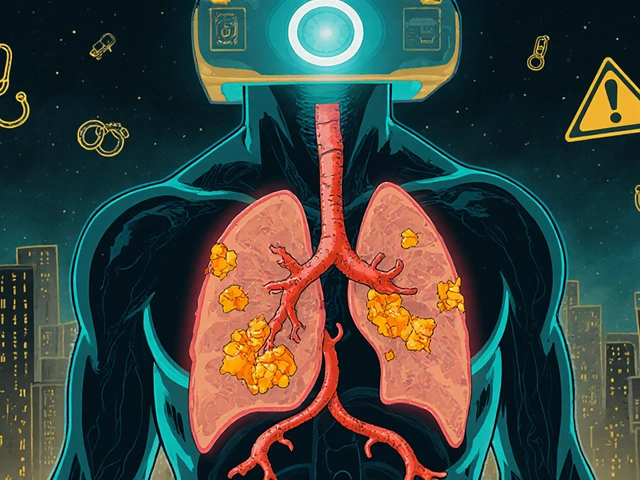
One of the most powerful allies in this effort is naloxone, an opioid antagonist that can reverse an overdose within minutes. Often carried by first‑responders, friends, and family, naloxone works by displacing opioids from brain receptors, restoring breathing. Its availability in pharmacies, community kits, and even schools has turned a once‑rare rescue drug into a standard safety net.
The drugs themselves matter, too. opioid analgesics, prescription pain relievers like oxycodone, hydrocodone, and morphine are essential for many patients but carry high overdose risk when misused or combined with sedatives. Understanding dosage limits, half‑life, and potential interactions—especially with benzodiazepines—helps clinicians write safer prescriptions and patients stay within safe limits.Beyond medication, systemic tools shape outcomes. Prescription Drug Monitoring Programs (PDMPs) track controlled‑substance prescriptions across providers, flagging risky patterns such as overlapping prescriptions or doctor‑shopping. When clinicians review a patient’s PDMP report, they can adjust therapy, offer counseling, or arrange addiction support before a dangerous escalation occurs.
Key Components of Effective Prevention
Harm‑reduction strategies complete the picture. Community‑run naloxone distribution sites, safe‑consumption spaces, and peer‑led education campaigns lower the odds that an accidental overdose goes untreated. Studies show that neighborhoods with robust harm‑reduction services see a measurable drop in overdose deaths, proving that prevention is as much about social infrastructure as it is about individual choice.
Education starts at the prescribing desk. Clinicians who discuss side‑effects, proper storage, and disposal of unused opioids reduce accidental ingestion by family members, especially children. Simple steps—locking medication cabinets, using take‑back programs, and avoiding sharing pills—cut down on unintentional exposure.
Patients and families also benefit from recognizing early overdose signs: pinpoint pupils, slowed breathing, blue‑tinged lips, or unresponsiveness. Promptly calling emergency services and administering naloxone, if available, can be the difference between life and death. Training workshops, often offered by local health departments, teach these skills in just a few hours.
Technology aids vigilance, too. Mobile apps now send reminders to refill prescriptions safely, alert users about dangerous drug‑drug interactions, and locate the nearest naloxone kit. Integrating these digital tools with traditional care creates a safety net that follows the patient wherever they go.
Finally, a supportive recovery environment matters. Connecting people who have experienced an overdose to counseling, medication‑assisted treatment (MAT), and peer support reduces the likelihood of repeat incidents. Programs that blend buprenorphine or methadone with counseling achieve higher retention rates, illustrating that medical treatment works best alongside psychosocial support.
All these pieces—naloxone access, careful prescribing, monitoring programs, community harm‑reduction, education, technology, and recovery services—form an interconnected system that makes opioid overdose prevention possible. Below you’ll find a curated collection of articles that dive deeper into each of these areas, offering practical advice, up‑to‑date research, and real‑world examples you can apply right away.
Naloxone Co-Prescribing: A Practical Guide to Overdose Prevention for Opioid Patients
Learn how naloxone co-prescribing works, when to use it, and practical steps for clinicians to prevent opioid overdoses. Includes risk factors, dosage calculations, formulation guide, and real‑world tips.