Corneal Thinning: Causes, Risks, and What You Need to Know
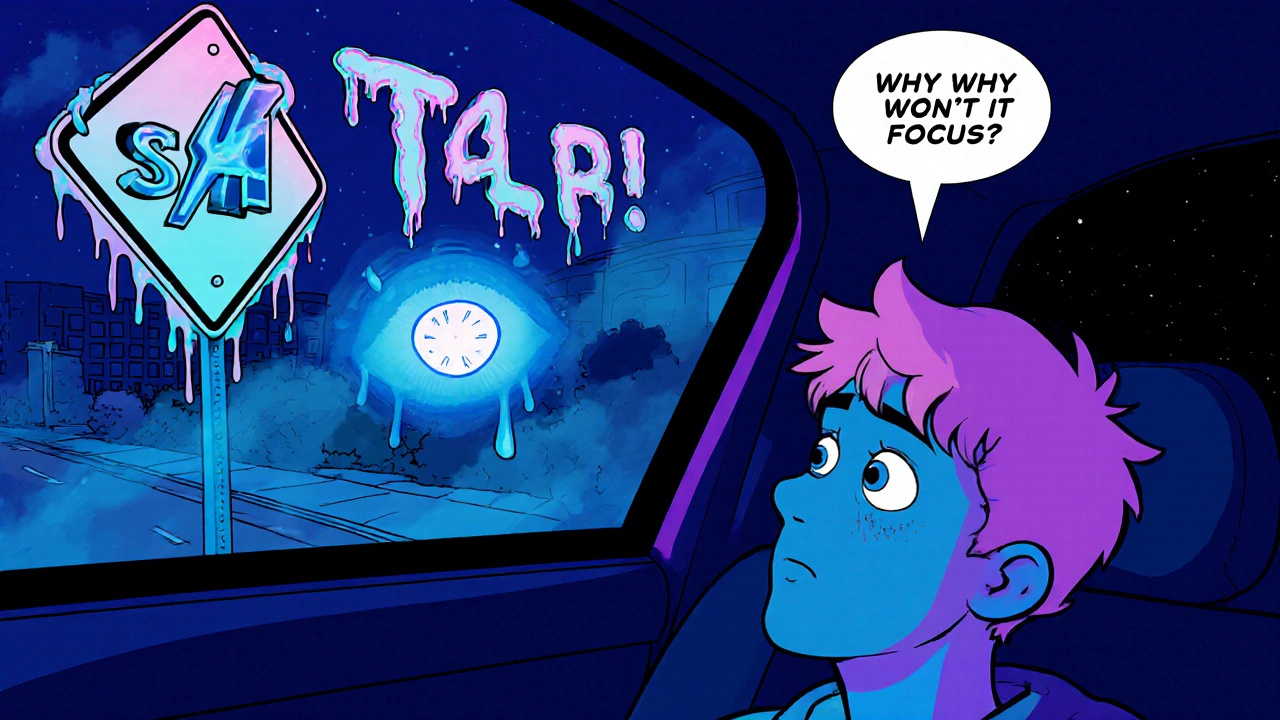
When the cornea, the clear front surface of the eye that helps focus light. Also known as the transparent outer layer of the eye, it plays a critical role in vision starts to thin, it doesn’t just weaken—it can change shape. This is corneal thinning, a condition where the cornea loses structural integrity and bulges outward, often leading to blurred or double vision. It’s not just a minor annoyance; left unchecked, it can progress to keratoconus, a progressive eye disease where the cornea thins and takes on a cone-like shape, which may require surgery if not managed early.
Corneal thinning doesn’t happen overnight. It’s often tied to chronic eye rubbing, genetic factors, or underlying conditions like allergies or connective tissue disorders. People who wear contact lenses for years, especially overnight lenses, are at higher risk. So are those with a family history of corneal problems. The real danger? Many don’t notice symptoms until vision is already affected. Mild cases might just mean needing stronger glasses. But as the cornea bulges, astigmatism gets worse, and contacts become uncomfortable or ineffective. That’s when corneal cross-linking, a minimally invasive procedure that strengthens the cornea using UV light and riboflavin becomes a game-changer. It’s not a cure, but it stops the thinning in its tracks for most patients.
What you won’t find in most brochures is how often this condition gets missed. Eye exams that only check vision with an eye chart won’t catch early corneal thinning. You need a topography scan—a detailed map of the cornea’s surface—to see the subtle changes. That’s why if you’ve noticed your vision changing slowly over months, or if your contacts feel like they don’t fit right anymore, it’s worth asking for this test. It’s quick, painless, and often covered by insurance. And if you’ve been told your vision problems are just "normal aging," push back. Corneal thinning can happen at any age, especially in teens and young adults.
The good news? We have more tools now than ever to manage this condition before it leads to vision loss. Beyond cross-linking, there are specialty contact lenses designed to reshape the cornea temporarily, and in advanced cases, transplants are highly successful. But catching it early is everything. The posts below cover everything from how to recognize the warning signs, to what medications or habits might make it worse, to real stories from people who’ve navigated treatment. You’ll find practical advice on protecting your eyes, understanding your diagnosis, and knowing when to ask for a second opinion. This isn’t just about eyesight—it’s about keeping your world clear for years to come.
Keratoconus: How Rigid Lenses Restore Vision When the Cornea Thins
Keratoconus causes progressive corneal thinning, leading to blurred vision. Rigid gas permeable and scleral lenses restore sight by creating a smooth optical surface over the irregular cornea, offering a non-surgical solution for most patients.