Brand Name Drugs: What They Are, Why They Cost More, and When They Really Matter
When you hear brand name drugs, the original versions of medications developed and marketed by pharmaceutical companies under a proprietary name. Also known as innovator drugs, they’re the first to hit the market after years of research and clinical trials. These are the pills you see advertised on TV—Lipitor, Cialis, Prozac—named after the company that made them, not the active ingredient. But here’s the thing: once the patent runs out, anyone can copy the formula. So why do brand name drugs still exist? And why do some people keep taking them even when cheaper generics are available?
The answer isn’t just about chemistry. It’s about patent exclusivity, legal protection that gives drug makers a temporary monopoly on selling their invention, and market exclusivity, a separate FDA rule that blocks generics from entering the market even after the patent expires, based on the company’s clinical data. Together, they can delay generics for over a decade. That’s why a drug like Humira stayed at $70,000 a year for years—even though its chemical formula was public. And that’s why some patients end up paying hundreds more per month just because their doctor or pharmacy didn’t suggest the generic.
But here’s where it gets real: for most people, generics work just as well. The FDA requires them to have the same active ingredient, strength, and absorption rate. So why do some folks stick with brand name drugs? In rare cases, it’s because of how the pill is made—the fillers, coatings, or release mechanisms. For drugs like seizure meds or thyroid hormones, even tiny differences can cause side effects or loss of control. One study found that switching from brand to generic levothyroxine caused noticeable changes in thyroid levels for 1 in 5 patients. That’s not common, but it’s enough to matter for someone who’s been stable for years.
Then there’s the psychological side. If you’ve been on a brand name drug for a long time, your body and mind get used to it. You trust the name. You remember the side effects you had before. You know what to expect. Switching to a generic can feel like rolling the dice—even if science says it’s safe. That’s why some doctors still prescribe brand name drugs for conditions like epilepsy, bipolar disorder, or chronic pain, even when the cost is a burden.
And let’s not forget the system. Pharmacy benefit managers, insurance formularies, and drug manufacturer rebates all play a role in what ends up on your shelf. Sometimes, the generic isn’t even offered because the brand pays the insurer to keep it off the list. Other times, you’re handed a brand name drug because your pharmacist didn’t ask if you’d prefer the cheaper version. It’s not always about what’s best—it’s about what’s easiest, cheapest, or most profitable.
What you’ll find below are real stories and practical guides from people who’ve navigated this maze. From how to ask your doctor about switching, to why some drugs just don’t play nice with generics, to how patent tricks keep prices high even after the science is old. You’ll learn when brand name drugs are worth the cost—and when you’re paying for a logo instead of better medicine.
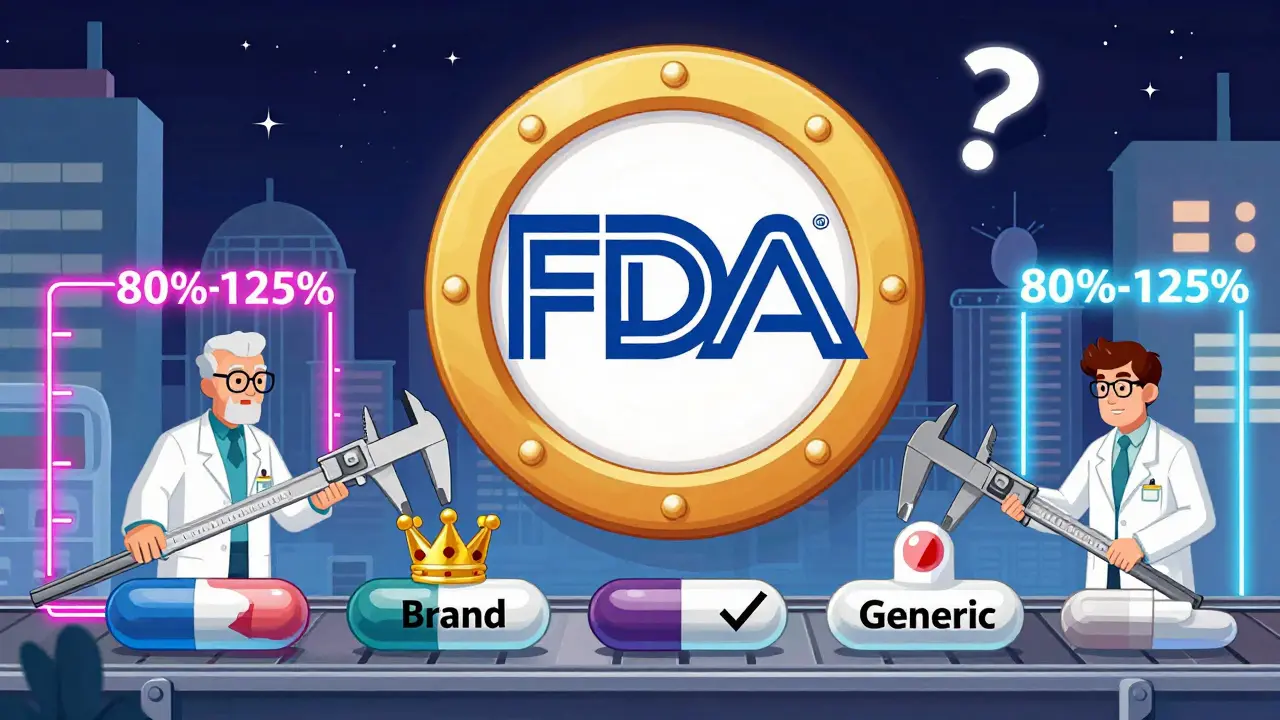
How the FDA Ensures Generic Drugs Work the Same as Brands
The FDA ensures generic drugs work the same as brand-name drugs through strict bioequivalence testing, identical active ingredients, and rigorous manufacturing standards. Over 90% of U.S. prescriptions use generics, saving billions annually.
How to Understand Authorized Generics and How They Differ from Traditional Generics
Authorized generics are the exact same drug as brand-name medications, just without the brand label. Learn how they differ from traditional generics in ingredients, cost, insurance coverage, and how to identify them.