Dental Anesthetic Selector
Recommended Anesthetic Agent
Onset: 2-3 mins
Duration: 1-2 hrs
Best For: Anterior teeth, routine work
Onset: 1.5-2 mins
Duration: 1-2.5 hrs
Best For: Posterior teeth, dense bone
Onset: 3-5 mins
Duration: 1-1.5 hrs
Best For: Quick recovery needed
Anesthetic Comparison Table
| Agent | Onset (mins) | Duration (hrs) | Penetration | Max Dose (mg/kg) |
|---|---|---|---|---|
| Lidocaine (1%) | 2-3 | 1-2 | Moderate | 7 (with epinephrine) |
| Articaine (4%) | 1.5-2 | 1-2.5 | High (especially dense bone) | 7 |
| Mepivacaine (2%) | 3-5 | 1-1.5 | Moderate | 6 |
When a dentist talks about "minimally invasive dentistry," the first thing most patients wonder is how painless it can be. The answer lies in local anesthesia. By numbing just the target area instead of the whole mouth, dentists can perform tiny, precise work while keeping patients comfortable and recovery times short. This article breaks down why local anesthesia is a game‑changer for modern dental practice, what drugs are most popular, how to choose the right technique, and what safety steps matter.
What is Local Anesthesia and Why It Matters
Local anesthesia a technique that temporarily blocks nerve transmission in a specific region of the body works by stopping pain signals at the source. In dentistry, that means the pulp, periodontal ligament, and surrounding soft tissue stay numb while the dentist drills, shapes, or restores a tooth. The benefit is twofold: the patient feels no pain, and the dentist can see the tooth clearly without strong reflexes that might mess up delicate work.
Minimally Invasive Dentistry Explained
Minimally invasive dentistry an approach that preserves as much natural tooth structure as possible while treating decay or damage relies on tiny cavities, laser or air‑abrasion tools, and conservative prep designs. The philosophy grew out of research showing that preserving enamel and dentin reduces long‑term fracture risk and keeps the tooth healthier. Because the work is so precise, any sudden movement from pain can ruin the outcome, which is why reliable anesthesia is essential.
Popular Dental Anesthetic Agents
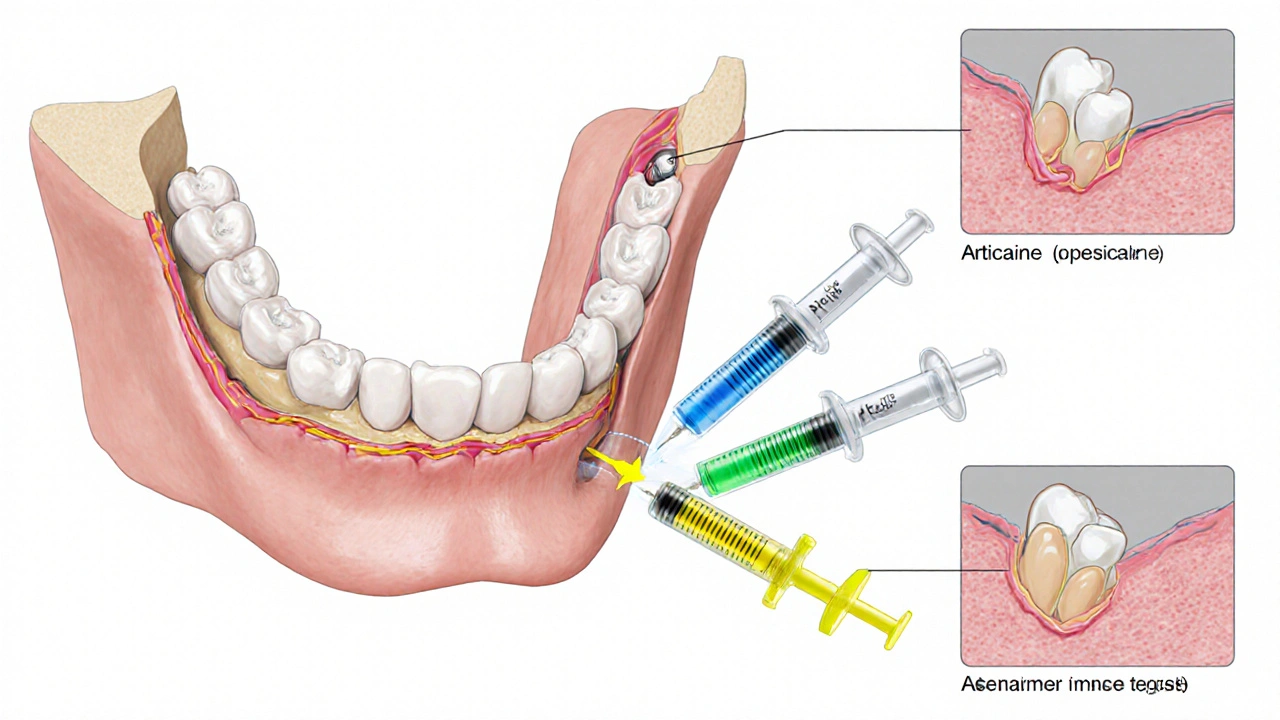
Not all anesthetic drugs behave the same. The three most common agents in the dental office are lidocaine, articaine, and mepivacaine. Each has a unique profile of onset, duration, and tissue penetration.
Lidocaine the classic amide anesthetic introduced in 1948, known for a rapid onset (2‑3 minutes) and moderate duration (1‑2 hours) remains a workhorse for both infiltration and nerve block techniques.
Articaine an amide with a thiophene ring that improves lipid solubility, giving a faster onset and deeper penetration, especially in dense bone is favored for posterior teeth where a stronger block is needed.
Mepivacaine an amide with a slightly longer onset (3‑5 minutes) but a shorter postoperative numbness, useful when a quick recovery of sensation is desired often appears in cases where patients need rapid clearance of the anesthetic effect.
Choosing the Right Technique
Two techniques dominate the field: infiltration anesthesia and the inferior alveolar nerve block. The choice depends on tooth location, bone density, and the planned procedure.
Infiltration anesthesia involves injecting the anesthetic directly into the tissue surrounding the target tooth and works best for front teeth and for patients with less cortical bone. It's quick, has a low risk of nerve injury, and provides excellent soft‑tissue control.
Inferior alveolar nerve block targets the mandibular nerve before it enters the mandibular canal, delivering numbness to all lower teeth on that side is the go‑to for molars and extensive work in the posterior mandible. While slightly more technique‑sensitive, it gives a broader field of anesthesia.
Safety: Adverse Reactions and Contraindications
Even though local anesthetics are safe, dentists must screen for allergies, cardiovascular issues, and drug interactions. The most common adverse reaction is a mild, temporary tingling or numbness that lasts beyond the procedure. Rarely, patients may experience systemic toxicity if the dose exceeds the maximum recommended limit (e.g., 7mg/kg for lidocaine with epinephrine).
Adverse reaction any unwanted physiological response to the anesthetic, ranging from local swelling to central nervous system toxicity requires immediate management, often with oxygen, airway support, and, if needed, a lipid emulsion therapy.
Contraindications include:
- Known allergy to amide anesthetics (e.g., lidocaine, articaine)
- Severe cardiac arrhythmias when using epinephrine‑containing solutions
- Pregnancy in the first trimester for high‑dose formulations
Impact on Patient Comfort and Clinical Outcome
When local anesthesia is applied correctly, patients report less anxiety, lower perceived pain scores, and quicker return to normal eating and speaking. For the clinician, a stable, pain‑free field means higher precision-critical for procedures like adhesive resin placement, micro‑preps for veneers, or laser cavity removal.
Studies from 2023‑2024 show that patients who received articaine infiltration for ClassI lesions in the premolar region reported a 30% reduction in pain intensity compared with lidocaine, while the overall procedure time dropped by 12% due to fewer interruptions.
Comparison of Common Dental Local Anesthetics
| Agent | Onset (minutes) | Duration (hours) | Peak Tissue Penetration | Typical Max Dose (mg/kg) |
|---|---|---|---|---|
| Lidocaine (1%) | 2‑3 | 1‑2 | moderate | 7 (with epinephrine) |
| Articaine (4%) | 1.5‑2 | 1‑2.5 | high (especially in dense bone) | 7 |
| Mepivacaine (2%) | 3‑5 | 1‑1.5 | moderate | 6 |
Practical Checklist for Dentists
- Confirm no amide‑type allergy; ask about past reactions.
- Choose anesthetic based on procedure depth and bone density (articaine for posterior mandible, lidocaine for routine anterior work).
- Calculate maximum dose using patient weight; keep a safety margin.
- Decide between infiltration and inferior alveolar nerve block according to tooth location.
- Document epinephrine concentration-usually 1:100,000 for most adult cases.
- Monitor patient for signs of systemic toxicity for at least 5minutes after injection.
- Provide post‑operative instructions on numbness duration and avoiding biting the cheek.
Frequently Asked Questions
Can I get a dental procedure done without any anesthesia?
Most patients need at least local anesthesia for any drilling or cutting. For ultra‑minimal procedures like a simple polishing, a dentist might use a topical numbing gel, but anything that penetrates dentin typically requires injection.
Is articaine safe for children?
Yes, but the dose must be reduced according to weight. Many pediatric guidelines recommend using lidocaine for younger children because of a slightly lower risk of paresthesia, while articaine is acceptable for those over 12 years with no allergy history.
How long does the numbness last after a filling?
Typical duration is 2‑4hours for lidocaine with epinephrine and 3‑5hours for articaine. The exact time varies with the amount injected and the individual’s metabolism.
What should I do if I bite my cheek while it’s still numb?
Rinse with cool water, apply a cold compress, and monitor for swelling. If the tissue looks damaged or you develop pain after the numbness wears off, contact your dentist.
Are there any alternatives to injectable anesthesia for minimally invasive work?
Topical gels, nitrous oxide (laughing gas), and oral sedatives can complement injections, but they rarely replace the need for local blocks when drilling or bonding deep cavities.
By aligning the right anesthetic agent, dose, and technique with the principles of minimally invasive dentistry, clinicians can deliver pain‑free, precise care that keeps patients coming back. The blend of modern anesthetic chemistry and conservative tooth preparation truly defines the future of dental practice.







katie clark
October 3, 2025 AT 21:25While the chemical nuances of lidocaine versus articaine are well‑documented, what truly distinguishes modern practice is the seamless integration of digital imaging with targeted anesthetic delivery, ensuring that conservatively prepared cavities remain truly minimally invasive.
Carissa Engle
October 6, 2025 AT 18:52Dental anesthetic selection has evolved from a one‑size‑fits‑all mindset to a patient‑centric algorithm that considers age weight bone density and procedural depth.
The clinician now consults a digital dosage calculator before drawing up any vial.
This safeguards against systemic toxicity while optimizing onset time.
Lidocaine remains the cornerstone for anterior restorations due to its moderate penetration and predictable duration.
Articaine, with its higher lipid solubility, excels in posterior extractions and dense mandibular bone where infiltration alone can suffice.
Mepivacaine offers a brief postoperative numbness, making it ideal for patients anxious about lingering cheek numbness.
The choice between infiltration and inferior alveolar nerve block hinges on the anatomical landscape of the target tooth.
Infiltration works best where cortical bone is thin, allowing rapid diffusion of the anesthetic.
Nerve block, though technique‑sensitive, provides comprehensive anesthesia for extensive molar work.
Epinephrine added to the solution prolongs vasoconstriction, thereby extending the anesthetic window.
However, patients with cardiovascular concerns require judicious epinephrine concentration.
Weight‑based dosing prevents exceeding the maximum milligram per kilogram threshold, a critical safety parameter.
Modern practice also emphasizes patient education on post‑procedure numbness to avoid inadvertent biting.
Documentation of the exact agent, dosage, and concentration has become a medico‑legal necessity.
Emerging technologies, such as computer‑controlled local anesthetic delivery, further refine the precision of infiltration.
Ultimately, the synergy of pharmacology and minimally invasive technique lifts patient comfort and procedural success to new heights.
Dervla Rooney
October 9, 2025 AT 16:18In addition to the pharmacokinetic profiles, clinicians should also assess the patient’s anxiety level and prior experiences with anesthesia, as these factors can influence perceived pain and cooperation during the procedure.
Understanding a patient’s medical history, especially any allergy to amide anesthetics, remains paramount.
Moreover, the selection of epinephrine concentration should be personalized to avoid excessive vasoconstriction in hypertensive individuals.
By adopting this holistic approach, the dentist can enhance comfort while maintaining safety.
Johnny Ha
October 12, 2025 AT 13:45Don’t let the dental board’s glossy brochures fool you-most of the “advanced” anesthetics are just a way for big pharma to line their pockets while the real trick is the practitioner’s skill, not the drug itself.
And if you’re not careful, you’ll end up with a numb jaw for half a day and still be wondering why the drill felt “painful”.
Hannah Dawson
October 15, 2025 AT 11:12The data tables you posted barely scratch the surface; a thorough breakdown would include not just onset and duration but also protein binding percentages and pKa values, which directly affect tissue diffusion rates.
Ignoring these metrics leads to suboptimal dosing, especially in patients with compromised hepatic metabolism.
Julie Gray
October 18, 2025 AT 08:38It is a known fact, though seldom advertised, that certain formulations of articaine have been linked in obscure studies to transient paresthesia in the lower lip when used for deep mandibular blocks.
Therefore, practitioners should exercise heightened vigilance when selecting agents for high‑risk procedures.
Lisa Emilie Ness
October 21, 2025 AT 06:05Use weight based calculations always avoid exceeding max dose
Emily Wagner
October 24, 2025 AT 03:32When we talk about the symbiosis of pharmacodynamics and minimally invasive protocols, we’re really discussing a paradigm shift that redefines patient‑centric care.
Think of the anesthetic as a catalyst that unlocks the potential of micro‑precision dentistry, allowing us to sculpt enamel with laser‑like accuracy.
Mark French
October 26, 2025 AT 23:58From a clinical perspective, it is essential to balance efficacy with patient comfort; however, many patients definately report residual numbness that interferes with everyday activities, such as drinking coffee or speaking clearly, which should be addressed in post‑operative instructions to ensure a smooth recovery and adequate patient satisfaction.
Daylon Knight
October 29, 2025 AT 21:25Oh great another table about lidocaine you’ve all seen a million times – because we totally needed more data on that.
Jason Layne
November 1, 2025 AT 18:52While the literature touts articaine as superior for posterior work, a closer inspection reveals that many studies suffer from selection bias, favoring outcomes that support pharmaceutical interests.
Consequently, dentists should critically evaluate the evidence before adopting it as a universal standard.
Vigilance is key to preserving clinical integrity.
Hannah Seo
November 4, 2025 AT 16:18Here’s a quick checklist for anyone planning a minimally invasive procedure:
1. Verify patient’s allergy status.
2. Calculate maximum dose based on weight.
3. Choose lidocaine for anterior work, articaine for dense bone.
4. Decide on infiltration vs. nerve block according to tooth location.
5. Document epinephrine concentration.
6. Monitor for toxicity post‑injection.
7. Give clear post‑op instructions on numbness and cheek protection.
Victoria Unikel
November 7, 2025 AT 13:45Patients often forget to avoid chewing on the numb side, which can lead to accidental injuries if not properly warned.
Lindsey Crowe
November 10, 2025 AT 11:12Wow, groundbreaking insights about numbing teeth.
Rama Hoetzlein
November 13, 2025 AT 08:38Analyzing the previous point, one must acknowledge that the omission of pharmacogenomic data undermines the entire dosing strategy, especially when considering polymorphisms in CYP2C9 that affect lidocaine metabolism 😊. Without this layer, clinicians are essentially operating blind, risking both under‑ and over‑anesthesia.
Dietra Jones
November 16, 2025 AT 06:05True, adding genotype info would make the dosage calculator far more robust and patient‑specific.
Victoria Guldenstern
November 19, 2025 AT 03:32It is amusing how the modern dental narrative romanticizes “precision” while ignoring the fact that most practitioners still rely on centuries‑old techniques for injection.
One could argue that the real “advancement” is simply better marketing for the same chemicals.
Nonetheless, the detailed breakdown of onset and duration does provide a useful reference for busy clinicians.
The emphasis on patient‑specific dosing is commendable, yet the average dentist rarely has time to calculate milligrams per kilogram on the spot.
Integration of digital calculators could bridge that gap, provided the software is user‑friendly.
Furthermore, the discussion of epinephrine concentrations reminds us that cardiovascular safety remains a priority.
Overall, the article balances technical detail with practical guidance, which is a rare achievement in dental literature.
Still, I would have liked to see more on emerging alternatives like liposomal anesthetic formulations.
Bill Bolmeier
November 22, 2025 AT 00:58Great rundown! I always make sure to double‑check the max dose and let my patients know they can’t bite their cheeks while the numbness lasts – it saves a lot of hassle later.
Danielle de Oliveira Rosa
November 24, 2025 AT 22:25The systematic presentation of the comparative table aids in quick decision‑making, especially when time pressures demand an immediate choice between lidocaine and articaine.
Tarun Rajput
November 27, 2025 AT 19:52In the grand tapestry of contemporary dental practice, the amalgamation of pharmacology and minimally invasive techniques weaves a narrative that is both scientifically rigorous and artistically nuanced.
The clinician, armed with a palette of anesthetic agents, must judiciously select the hue that best complements the patient’s unique physiological canvas.
Understanding the subtle interplay between onset velocity and tissue penetration allows for a choreography that minimizes discomfort and maximizes efficiency.
When confronting dense mandibular bone, the high lipid solubility of articaine becomes the virtuoso, delivering profound anesthesia where lidocaine merely whispers.
Conversely, for delicate anterior restorations, the modest yet reliable profile of lidocaine ensures elegance without over‑indulgence.
Weight‑based dosing is the metronome that keeps the performance from spiraling into toxicity, a reminder that precision is paramount.
Incorporating epinephrine in measured doses acts as a tempo‑setter, extending the anesthetic’s resonance while safeguarding hemodynamic stability.
Post‑operative guidance, such as avoiding cheek biting during the numb phase, serves as the final crescendo, ensuring patient safety after the curtain falls.
Thus, the synthesis of these elements culminates in a symphony of patient‑centered care that resonates long after the dental chair is vacated.
Ultimately, mastery lies not just in the drugs themselves, but in the clinician’s ability to orchestrate them with finesse.