When someone overdoses, every second counts. But calling the wrong number could cost them their life. You might think calling 911 is always the right move - and sometimes it is. But in other cases, calling Poison Control first can save time, money, and even lives. The key isn’t guessing. It’s knowing the signs.
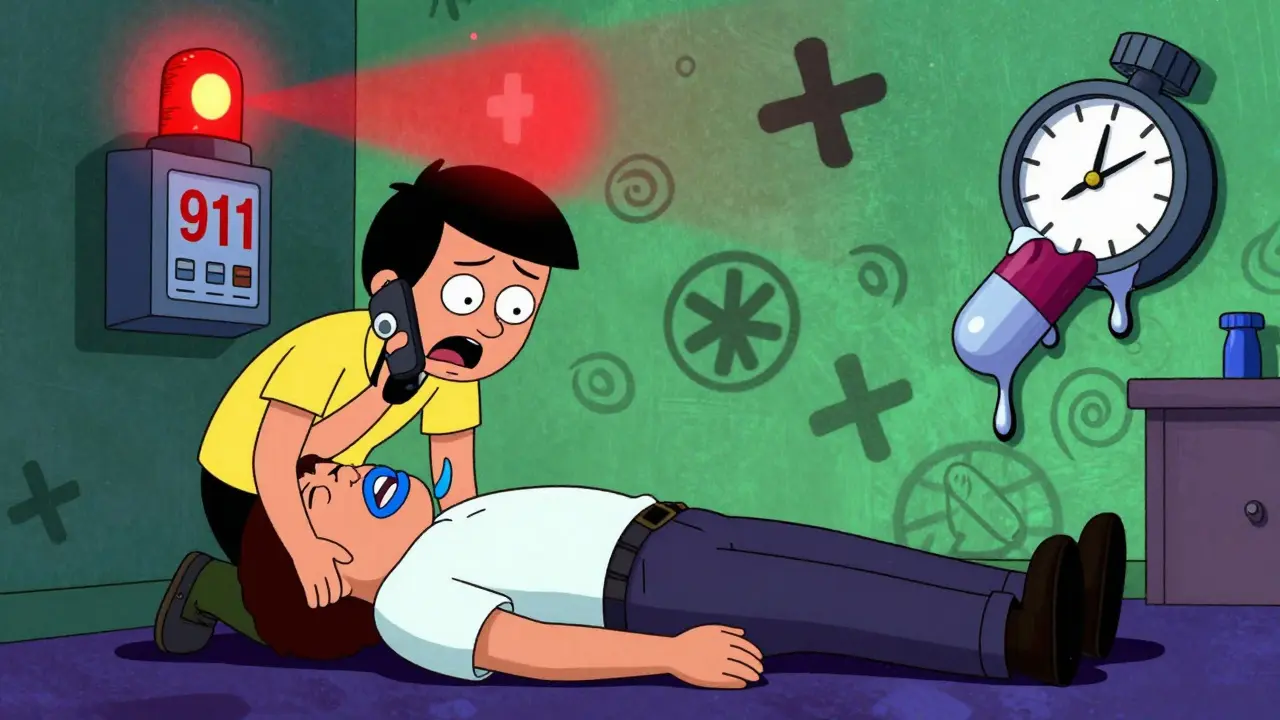
Call 911 Immediately If They’re Unresponsive or Struggling to Breathe
If the person is not waking up, has blue lips or fingertips, or is gasping for air, don’t hesitate. Dial 911 right away. These aren’t vague warning signs - they’re life-or-death signals. According to CDC data, 28.3% of fatal poisoning cases involve respiratory failure. If someone can’t breathe, their brain is already being starved of oxygen. Waiting to call Poison Control first could mean the difference between survival and death.Same goes for seizures lasting more than five minutes, or if their heart is racing uncontrollably or their blood pressure has dropped below 90. These are signs of cardiovascular collapse. Even if they seem okay five minutes ago, drugs like fentanyl, certain heart medications, or synthetic opioids can shut down the body in under 15 minutes. Emergency responders carry naloxone, oxygen, and IV fluids - tools Poison Control can’t send. If you suspect an opioid overdose, give naloxone if you have it, then call 911. Don’t wait to see if it works.
Poison Control Is Your Best Bet for Stable, Asymptomatic Cases
Not every overdose is an emergency. Sometimes, someone accidentally takes two pills instead of one. Or a child grabs a bottle of vitamins. If the person is awake, breathing normally, talking clearly, and has no symptoms - then Poison Control is the right first step.They handle about 2.1 million cases a year in the U.S., and 82% of pediatric exposures under age six are safely managed with their guidance. For adults, if it’s a single substance - like an extra dose of ibuprofen or a missed dose of blood pressure medication - and they’re acting normal, Poison Control can tell you whether to watch and wait, or head to the ER. They know the exact toxic dose for hundreds of medications. A 150 mg/kg acetaminophen overdose in a healthy adult? That’s a hospital trip. But 120 mg/kg? They might tell you to drink water, monitor for nausea, and check liver enzymes in 24 hours.
They also know how formulations matter. An extended-release oxycodone pill is far more dangerous than the immediate-release version, even if the milligram amount is the same. Poison Control specialists can tell you that. ER doctors can’t always access that detail in the first five minutes.
What Information Do You Need Before You Call?
Whether you’re calling Poison Control or 911, having the right info ready saves critical minutes. Don’t waste time searching for bottles while someone is slipping away. Keep this list handy:- Exact name of the substance - including brand and generic name
- Strength and form - tablet, liquid, patch, extended-release?
- How much was taken - in milligrams or milliliters, not "a handful"
- When it happened - even within 15 minutes helps
- Person’s weight in kilograms - yes, this matters for dosing
- Current symptoms and when they started
- Any first aid already given - like vomiting, activated charcoal, or naloxone
Keep the pill bottle nearby. If you can’t find it, take a photo. Poison Control uses the label to identify hidden ingredients - like acetaminophen mixed into painkillers, which can cause silent liver damage. A 2022 study found that 27% of home estimates of ingested amounts are off by more than 10%. That’s enough to change the entire response.

Special Cases: Kids, Seniors, and Carbon Monoxide
Children under six account for nearly half of all Poison Control calls. But not all are equal. If a toddler swallows one aspirin, Poison Control may say: "Watch for vomiting, call back if they seem sleepy." But if they swallow even half a clonidine pill (used for ADHD or high blood pressure), that’s a 911 call. Toxic dose? Just 0.01 mg/kg. One pill can drop their blood pressure and heart rate to dangerous levels.Seniors over 75 are another high-risk group. On average, they take five or more medications daily. Even a small overdose of a blood thinner or diabetes drug can spiral fast. A 2022 JAMA study found 83% of adults over 75 take five or more prescriptions. Interactions can be unpredictable. If a senior takes too much of anything - even something they’ve taken for years - get them to the ER. Don’t wait.
Carbon monoxide poisoning is different. Even if someone feels fine - just a headache or dizziness - call 911 immediately. Carbon monoxide has no smell, no taste, and symptoms can seem mild at first. But 42.7% of people who seem okay at first develop serious brain damage hours later. Poison Control will tell you to get out of the house and call 911. No exceptions.
Why Not Just Always Call 911?
It’s tempting. But calling 911 for every small exposure clogs up the system. Emergency crews are stretched thin. In 2022, 4.7% of all 911 calls were for suspected poisoning - and many were unnecessary. A Connecticut Poison Control Center study found that when families called Poison Control first, unnecessary ER trips dropped by 38.6%. That means ambulances and ER beds are free for people who truly need them.Plus, Poison Control gives you real-time, personalized advice. They’ll tell you whether to induce vomiting (usually no), give activated charcoal (only if it’s safe and timely), or just watch. ERs can’t always offer that level of detail in the chaos.

What About the Poison Control App or Website?
The webPOISONCONTROL tool and mobile app are useful - but they’re not a replacement for a live expert. They work great for stable, single-substance exposures in healthy adults. But if someone is already showing symptoms, has taken multiple drugs, or it’s an intentional overdose - you must call the hotline directly. The app can’t assess breathing, consciousness, or heart rhythm.Also, the app doesn’t connect you to a specialist. It gives general advice. In one 2023 FDA review, 18.3% of app users thought they could manage a high-risk overdose at home - and ended up in the ER anyway. Use the app to prepare info before calling, not instead of calling.
Language Barriers and Access
Only 17 of the 55 Poison Control centers offer real-time Spanish interpretation. Just three offer Mandarin. That’s a problem in a country where nearly a quarter of households speak a language other than English at home. If you’re not fluent in English, don’t wait to find someone who can translate. Call 911. Emergency responders are trained to handle language barriers - they have access to interpreters instantly. Poison Control may not.Final Rule: When in Doubt, Call 911
There’s no shame in overreacting. If you’re unsure - if your gut says something’s wrong - call 911. It’s better to have a false alarm than a tragedy. But if the person is stable, alert, and you know what was taken, call Poison Control first. They’re free, fast (average answer time: 28 seconds), and trained to handle exactly this.The system works best when you know the difference. Not every overdose needs sirens. But every life-threatening overdose needs help - now.
Can I call Poison Control for a suspected drug overdose?
Yes - but only if the person is awake, breathing normally, and has no symptoms. If they’re unconscious, having seizures, or struggling to breathe, call 911 immediately. Poison Control is best for stable, single-substance exposures where the amount and time are known.
Is Poison Control free and confidential?
Yes. The Poison Help hotline (1-800-222-1222) is free, confidential, and available 24/7. No insurance or ID is required. It’s funded by federal grants and operates through regional centers across the U.S.
What should I do if I suspect an opioid overdose?
Give naloxone if you have it, then call 911 immediately. Even if naloxone brings them back, synthetic opioids like fentanyl can wear off before the drug does, causing a second overdose. Emergency responders can provide ongoing care and transport to the hospital.
Can I use the Poison Control app instead of calling?
The app is useful for gathering info or checking general risks, but it doesn’t replace a live specialist. If someone has symptoms, took multiple substances, or is a child or senior, always call the hotline. The app can’t assess breathing, consciousness, or heart rate.
Why do I need to know the person’s weight?
Toxicity is calculated by weight - milligrams per kilogram. A 10-year-old and a 200-pound adult can have completely different reactions to the same dose. Guessing weight leads to dangerous errors. If you don’t know it, estimate as accurately as possible - it’s better than nothing.
What if I’m not sure what was taken?
Call 911. If you can’t identify the substance and the person has symptoms, assume it’s serious. Emergency responders can test blood and urine on-site. Poison Control needs specifics to help - if you don’t have them, the ER is safer.
Do I need to go to the ER after calling Poison Control?
Sometimes. Poison Control will tell you whether to monitor at home or go to the ER. If they say "go," go immediately. Don’t wait for symptoms to worsen. Some drugs cause delayed damage - like liver failure from acetaminophen - that doesn’t show up for hours.
Can Poison Control help with alcohol overdoses?
Yes, but only if the person is conscious and breathing. Severe alcohol poisoning causes vomiting, seizures, slow breathing, and unconsciousness - all signs to call 911. Poison Control can advise on mild cases, like someone who drank too much but is alert and stable.






Damario Brown
January 15, 2026 AT 11:48just called poison control last week after my kid ate half a bottle of gummy vitamins. they told me to watch for vomiting and check in 4 hours. no hospital, no cost. these people are unsung heroes. if you think they’re just a hotline, you’ve never been on the line with someone who knows exactly how much acetaminophen turns your liver into a brick.
Robin Williams
January 15, 2026 AT 13:00life’s not a flowchart. sometimes you just gotta trust your gut. i once thought my buddy was just "feeling weird" after mixing benzos and energy drinks. he was fine. until he wasn’t. 911 saved his life. poison control’s great for the small stuff, but when your brain says "this is wrong," don’t overthink it. call 911. always.
Anny Kaettano
January 17, 2026 AT 00:14as a nurse who’s seen too many preventable deaths, i can’t stress this enough: knowing the exact dose matters more than you think. i had a patient last month who took "a couple" of melatonin gummies. turned out it was 30mg - that’s like 15x the adult dose. poison control caught it because we had the bottle. keep the container. take a pic. don’t guess. your life - or someone else’s - could depend on it.
Kimberly Mitchell
January 17, 2026 AT 18:48why are we still talking about this like it’s a new concept? people have been overdosing since aspirin was invented. if you can’t tell the difference between a minor mistake and a life-threatening emergency, maybe you shouldn’t be around medications at all. stop making this into a public service announcement. take responsibility.
Trevor Davis
January 19, 2026 AT 16:23man i love how poison control is this quiet superhero. no capes, no fanfare. just a calm voice on the phone telling you whether your kid’s gonna be okay after eating a whole bag of gummy worms. i used to think they were just a glorified google search. now? i keep their number on my fridge. next to the fire extinguisher.
John Tran
January 20, 2026 AT 01:26think about it: our entire modern relationship with medicine is built on a paradox. we’re told to trust science, but when it comes to our own bodies, we’re left to guess. we’re given pills with no context, no education, no manual - then we panic when something goes wrong. poison control isn’t just a service - it’s a philosophical counterweight to a system that treats human biology like a vending machine. we’ve outsourced our intuition to pharmaceutical marketing and now we’re paying the price in ER bills and dead toddlers. the real tragedy isn’t the overdose - it’s that we didn’t teach people how to think before they swallowed.
mike swinchoski
January 21, 2026 AT 13:24you people are idiots. if you don’t know what’s in that pill, don’t take it. simple. if your kid eats something, you’re a bad parent. poison control is for people who can’t parent. 911 is for people who can’t think. stop making excuses. just be responsible.
Gregory Parschauer
January 22, 2026 AT 00:16you’re all missing the point. this isn’t about calling the right number - it’s about systemic neglect. why does a 7-year-old in rural Alabama need to wait 12 minutes for poison control because their center is understaffed? why are we relying on volunteers with outdated databases? this isn’t a guide - it’s a bandaid on a severed artery. fix the infrastructure, not the advice.
Trevor Whipple
January 22, 2026 AT 17:24lol you think poison control can handle fentanyl? please. they don’t even know what carfentanil is. i work in EMS. we get called for "suspected overdose" and it’s always some guy who took 3 oxycodone and thinks he’s fine. they give him advice. he dies in the car. call 911 every time. period. end of story.
Milla Masliy
January 24, 2026 AT 07:13my mom’s from Mexico and she didn’t speak English. when her neighbor’s grandkid swallowed a button battery, she called 911 right away. the paramedics had an interpreter on standby. no hesitation. no waiting. that’s the real lesson here - if you’re not 100% sure, go with the system that’s built to handle chaos. poison control is great - but 911 doesn’t need a translator.
Clay .Haeber
January 25, 2026 AT 22:54so let me get this straight - we’ve got a national hotline staffed by toxicologists who can tell you the exact lethal dose of NyQuil… but you’re supposed to wait for them to answer while your cousin is turning blue? genius. next you’ll tell me to use a compass to find the ER. call 911. always. poison control is for people who like to read the manual before the fire starts.