For millions of people struggling with insomnia, the first solution that comes to mind is a pill. A quick fix to shut off the racing mind and fall asleep. But what if the real answer isn’t in a bottle, but in your thoughts, habits, and bedtime routine? Cognitive Behavioral Therapy for Insomnia - or CBT-I - isn’t just another option. It’s the most proven, lasting solution doctors now recommend before any medication.
Why Sleep Medications Don’t Solve Insomnia
Sleep medications like zolpidem (Ambien) work fast. You take them, you feel drowsy, and you fall asleep. But they don’t fix the problem. They just mask it. And the longer you use them, the less they work. Studies show that 42% of people develop tolerance to these drugs within eight weeks. That means you need more to get the same effect. Then come the side effects: morning grogginess, memory lapses, dizziness, even increased fall risk in older adults. The FDA has flagged these risks for years, yet prescriptions keep climbing - zolpidem alone made up nearly half of all insomnia prescriptions in the U.S. in 2022. The bigger issue? When you stop taking the pill, insomnia often comes back worse than before. That’s because medications don’t change the underlying causes: the anxious thoughts about not sleeping, the habit of lying awake for hours, the body’s constant state of alertness. They treat the symptom, not the system.What CBT-I Actually Does
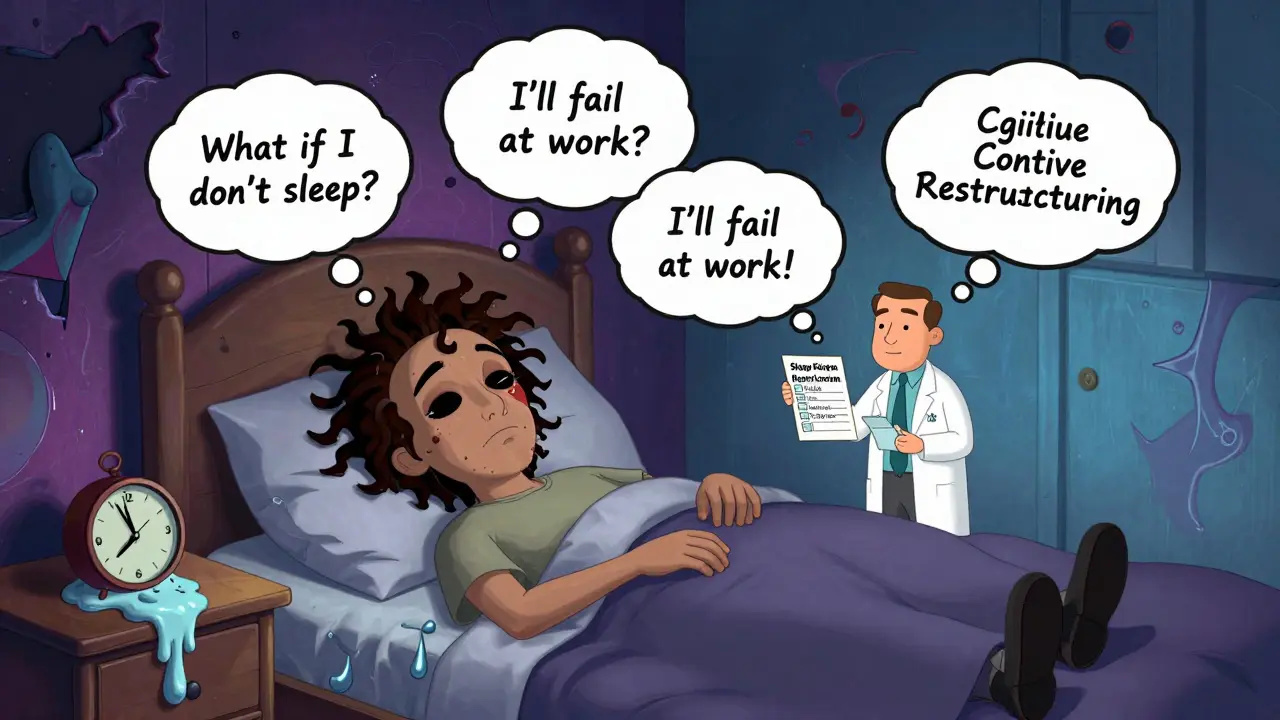
CBT-I is a structured, science-backed program designed to rewire how you think and behave around sleep. It’s not hypnosis. It’s not meditation. It’s a set of specific, measurable techniques taught over 6 to 8 weekly sessions. Each one targets a different part of the insomnia cycle. The core of CBT-I isn’t one trick - it’s five tools working together:- Sleep Restriction: You spend less time in bed - even if you’re tired. If you only sleep 5 hours a night, you’re only allowed 5 hours in bed. It sounds cruel, but it forces your body to build strong sleep pressure. Within weeks, sleep efficiency jumps. Studies show this single technique accounts for nearly 40% of CBT-I’s success.
- Stimulus Control: Your bed is only for sleep and sex. No scrolling, no watching TV, no lying there worrying. If you’re awake for more than 20 minutes, you get up and go to another room until you feel sleepy. This breaks the mental link between your bed and frustration.
- Cognitive Restructuring: You challenge the catastrophic thoughts: “If I don’t sleep 8 hours, I’ll fail at work.” “I’ll never recover from this.” Therapists help you replace these with facts: “My body still repairs itself on 6 hours.” “Insomnia is treatable.” People who completed 80% of these exercises saw 62% greater improvement than those who didn’t.
- Relaxation Training: Breathing exercises and muscle relaxation reduce the physical tension that keeps you awake. Polysomnography data shows a 27% drop in hyperarousal markers after just six weeks of daily practice.
- Sleep Hygiene: Not just “avoid caffeine.” It’s about consistent wake times (even on weekends), avoiding bright screens before bed, keeping the bedroom cool and dark, and not napping after 3 p.m.
The Evidence Is Clear: CBT-I Wins in the Long Run
In the first 4 to 8 weeks, sleep meds and CBT-I look about equal. Both help you fall asleep faster and stay asleep longer. But after that, the gap widens - dramatically. A 2023 study of over 4,000 people found that at six months, those who did CBT-I had a 3.2-point greater improvement on the Insomnia Severity Index than those on medication. At one year, 68% of CBT-I patients were still sleeping well. Only 32% of medication users were. And it gets better. A 2023 study tracked patients for over a decade. Those who completed CBT-I still had significantly better sleep than before treatment - even 10 years later. That’s not possible with pills. Medications don’t build lasting skills. CBT-I does. Even better? Digital versions work just as well. Platforms like Sleepio and Somryst, approved by the FDA as prescription digital therapeutics, have helped over 140,000 Medicare patients since 2022. One Reddit user, u/SleepWarrior89, said after six weeks of strict sleep restriction: “My sleep efficiency went from 68% to 92%. The hardest part? Sticking to my wake-up time on weekends.”
Why Isn’t Everyone Doing CBT-I?
If it’s so effective, why aren’t more people getting it? The answer is simple: access and cost. Only 15% of U.S. primary care doctors feel trained to deliver CBT-I. Most don’t know how to refer patients. Insurance often covers a $15 zolpidem prescription but only pays $120 per CBT-I session - and many plans don’t cover it at all. In the UK, NHS access is patchy. Private therapy can cost £80-£150 per session. That’s why digital CBT-I is changing everything. You can now do the full program at home, on your phone, for under £50. Studies show 65-70% of people complete digital CBT-I - just like in-person. Older adults, who struggle with tech, still succeed when programs are simplified. One 2024 trial found 82% of adults aged 65-85 completed tailored digital CBT-I with just 15 minutes a day.Who Benefits Most?
CBT-I works for almost everyone with chronic insomnia - whether you’re 22 or 72. But it’s especially powerful for groups often overlooked:- Adolescents: A 2024 meta-analysis found CBT-I improved sleep onset by nearly 30 minutes and added over 45 minutes of sleep - while medications showed no lasting benefit.
- Cancer survivors: Nearly half suffer from insomnia. CBT-I helps without interfering with treatment.
- Pregnant women: Medications are risky. CBT-I is safe and effective.
- People with anxiety or depression: CBT-I often improves mood too, because poor sleep fuels mental health struggles.

What to Expect - and What to Avoid
Starting CBT-I isn’t easy. The first two weeks are the hardest. Sleep restriction means you’ll be tired. You might feel worse before you feel better. That’s normal. The key is sticking with it. Avoid these pitfalls:- Trying to “catch up” on sleep by napping or sleeping in - it breaks the rhythm.
- Checking the clock every 10 minutes - it fuels anxiety.
- Using alcohol to fall asleep - it fragments sleep later in the night.
- Waiting until you’re “exhausted” to go to bed - that’s when your brain starts racing.
The Future of Sleep Treatment
The sleep medicine world is shifting. In 2020, Somryst became the first FDA-approved digital CBT-I therapy. In 2022, Sleepio followed. Now, 17 platforms are in clinical validation. AI is being used to personalize sleep restriction schedules - making them even more effective. Medicare and major insurers like UnitedHealthcare now cover digital CBT-I. Over 60 Fortune 500 companies offer it through employee wellness programs. This isn’t a trend - it’s a new standard. The message is clear: if you’ve been struggling with sleep for more than a few months, a pill isn’t your best bet. CBT-I is. It takes effort. It takes time. But the results? They last.Is CBT-I better than sleeping pills?
Yes, for chronic insomnia. While sleeping pills work faster in the short term, CBT-I provides lasting results without side effects. Studies show 68% of people who complete CBT-I still sleep well a year later, compared to just 32% of those who used medication. CBT-I treats the root causes - not just the symptoms.
Can I do CBT-I on my own?
Yes, with the right digital tools. Platforms like Sleepio and Somryst are designed for self-guided use and have success rates matching in-person therapy. They include step-by-step lessons, sleep diaries, and progress tracking. However, working with a trained therapist can help if you’re struggling with anxiety or have complex health conditions.
How long does CBT-I take to work?
Most people start seeing improvements in 2 to 4 weeks. The biggest changes - like falling asleep faster and waking up less - usually happen between weeks 4 and 8. The key is consistency. Skipping sessions or giving up too soon reduces effectiveness. The full program typically lasts 6 to 8 weeks.
Does CBT-I work for older adults?
Absolutely. In fact, older adults often benefit more than younger people because they’re more likely to have developed poor sleep habits over time. Digital CBT-I programs tailored for seniors have a completion rate of 82%, even with minimal tech support. No medication side effects make it safer for those on multiple prescriptions.
What if I can’t stick to sleep restriction?
It’s the hardest part - and the most common reason people quit. If you’re struggling, talk to your therapist or adjust the protocol slightly. Some programs start with less restriction and build up. The goal isn’t perfection - it’s progress. Even partial adherence improves sleep. Don’t give up after one tough week.
Is CBT-I covered by insurance?
In the U.S., Medicare and many private insurers like UnitedHealthcare now cover digital CBT-I under CPT code 96156. In the UK, NHS access is limited, but private providers and employee wellness programs often cover it. Always check with your insurer - coverage is expanding rapidly.




Henry Jenkins
January 27, 2026 AT 17:43Man, I tried Ambien for like three months after my divorce. Fell asleep fast, but woke up feeling like I’d been hit by a bus. Then I tried CBT-I through Sleepio-no pills, just discipline. First two weeks? I was a zombie. But by week five, I was sleeping 7 hours straight without even thinking about it. Now I don’t even keep pills in the house. It’s not magic, it’s just rewiring. And yeah, it’s harder than popping a pill, but worth every sleep-deprived night.
Also, the sleep restriction thing? Brutal at first. But once your body realizes you’re not lying there wasting time, it starts cooperating. Like your brain finally goes, ‘Oh, you’re serious about this.’
Dan Nichols
January 28, 2026 AT 22:19CBT-I is just placebo with a syllabus. Everyone knows pills are addictive but they work. You think people are gonna sit there doing breathing exercises when they’ve got deadlines and kids and anxiety? No. They want a damn solution not a lecture. The fact that 42% develop tolerance means the meds are working too well to be safe. And you call that a fix? I call it a trap. CBT-I is for people who have time to waste. I’ve got a life to live.
Also 68% still sleeping well after a year? Where’s the control group? Who funded this study? Big sleep tech?
And don’t get me started on digital apps. My grandma can’t even turn off her phone.
Stop selling snake oil as science.
Renia Pyles
January 30, 2026 AT 13:04Ugh I HATE when people act like CBT-I is some holy grail. I did it. I did the whole damn program. Woke up at 5am every day for two weeks. Wrote in my stupid sleep diary. Sat in a dark room staring at the ceiling like a lunatic. And guess what? I still wake up at 3am thinking about my ex. The therapy didn’t fix my trauma. It just made me feel guilty for not being ‘fixed’ enough. So now I take a low dose of trazodone and I’m actually happy. Why is everyone so obsessed with ‘natural’ solutions? Because they don’t want to admit that sometimes, you need chemicals to survive.
And yes I’m tired of being told I’m weak because I use meds. I’m not weak. I’m tired.
Karen Droege
January 30, 2026 AT 21:47Okay I need to scream into the void because I’ve been on both sides and I’m here to tell you-CBT-I is the goddamn answer. I was a 45-year-old mom of three, surviving on 3 hours of sleep and 2 cups of coffee. My doctor handed me Ambien like it was Advil. I took it for 11 months. Then my anxiety spiked, my memory went haywire, and I almost fell down the stairs. That was my wake-up call.
I did Sleepio. I cried. I failed. I got mad. I stuck with it. And now? I sleep like a baby. No meds. No guilt. Just rhythm. And let me tell you, the sleep restriction part? It’s not cruel-it’s a reset. Your body isn’t broken, it’s confused. CBT-I is the therapist that whispers, ‘Hey, remember how to sleep?’
Also, if you’re an older adult or a cancer survivor or a pregnant woman-this isn’t ‘alternative.’ This is survival. And yes, digital versions work. My 71-year-old dad did it on his iPad. He didn’t even know what ‘stimulus control’ meant. He just followed the app. Now he’s sleeping 7 hours. I cried. Again.
Stop listening to the naysayers. Your brain deserves better than a chemical crutch.
Napoleon Huere
January 31, 2026 AT 04:30It’s funny how we treat sleep like a problem to be solved instead of a natural state to be restored. We’ve turned our bedrooms into war zones-glowing screens, caffeine bombs, anxiety loops-and then we’re shocked when we can’t rest.
Medication is the modern equivalent of slapping a bandage on a broken leg and calling it healed. CBT-I doesn’t just treat insomnia-it teaches you how to live again. It’s not about ‘fixing’ sleep. It’s about reclaiming the biological rhythm we’ve been trained to ignore.
Think about it: we don’t medicate hunger. We don’t give pills to people who can’t breathe fresh air. We fix the environment. Why is sleep any different?
Maybe the real epidemic isn’t insomnia-it’s the belief that we can outsource our biology to a pill.
Also, if you’re 22 and scrolling TikTok till 2am, no pill will save you. You need to turn off the damn phone.
Aishah Bango
January 31, 2026 AT 09:35People who take sleeping pills are just lazy. If you can’t fix your sleep with discipline, then you’re not trying hard enough. I’ve been doing CBT-I for six weeks and I haven’t had a single pill. I don’t even drink coffee after noon. I go to bed at 10:30. I don’t check my phone. I meditate. I journal. I’m not some saint-I’m just responsible. And if you can’t do the same, maybe your insomnia isn’t medical-it’s moral.
Also, digital apps are just a crutch for people who can’t follow basic instructions. If you need an app to tell you to sleep, you’ve already lost.
Peter Sharplin
February 1, 2026 AT 09:05Just wanted to say-this post is spot on. I’m a therapist who specializes in CBT-I and I see this every day. People come in desperate, blaming themselves. ‘I’m broken.’ ‘I’m weak.’ But the truth? Your nervous system is just stuck in fight-or-flight mode. CBT-I doesn’t fix your mind-it calms your body.
And yeah, sleep restriction sucks. But it’s like physical therapy after a knee injury. You’re not supposed to feel good at first. You’re supposed to rebuild.
Also, the 68% success rate after a year? That’s not just data-that’s people getting their lives back. I had a veteran who hadn’t slept through the night in 12 years. After CBT-I? He started playing guitar again. He said he forgot what it felt like to wake up not afraid.
Don’t let the noise drown out the science. This works. And it’s not magic. It’s medicine.
shivam utkresth
February 3, 2026 AT 06:38Bro in India we don’t even have access to this. My cousin had insomnia for 5 years. Doctor gave him zolpidem. He took it for 2 years. Now he’s on antidepressants because the pills messed up his serotonin. No CBT-I here. No Sleepio. No insurance coverage. Just ‘take this, sleep better.’
But I read this whole thing and I’m gonna try it myself. I’m 28, work from 8am to 11pm, and my brain never shuts off. Maybe I’ll start with just one thing-no phone after 11pm. Baby steps.
Also, I love how you said ‘sleep hygiene’ isn’t just ‘no caffeine.’ That’s the problem. Everyone thinks it’s about tea and lavender. Nah. It’s about boundaries. And we don’t have those here. We just burn out.
John Wippler
February 4, 2026 AT 09:58Let me tell you something. I used to be the guy who slept 2 hours and then said ‘I’m fine.’ I thought I was a productivity ninja. Turns out I was just running on fumes. My body started shutting down-heart palpitations, brain fog, panic attacks. I thought I was stressed. Turns out I was sleep-deprived.
I did CBT-I. I cried in week 3. I wanted to quit. But I didn’t. And now? I’m not just sleeping-I’m *resting*. My anxiety dropped 70%. My creativity came back. I started writing again.
Look, I’m not saying this is easy. But I’m saying it’s worth it. You’re not lazy. You’re not broken. You’re just tired. And your body is begging you to listen.
Start small. One week. One rule. No screens after 10. Then build. You’ve got this. I believe in you.
Faisal Mohamed
February 5, 2026 AT 04:21CBT-I is the new spiritual awakening for the algorithm generation 🤓🌙
We’ve traded transcendence for sleep efficiency metrics. Now we track REM cycles like they’re crypto gains. I’m not mad. I’m just… intrigued. Is this the next phase of human optimization? No pills. No gurus. Just a phone app telling you to ‘get out of bed if you’re not asleep in 20 mins.’
It’s beautiful. And terrifying.
Also, my dog now sleeps on my pillow because I stopped letting him in at 11pm. He’s judging me. But I’m winning. 🐶💤
Josh josh
February 6, 2026 AT 19:56i tried the sleep thing and it worked but i still wake up at 3am and think about my ex and then i scroll for an hour and then i feel guilty and then i fall asleep at 6am and its like a loop and i dont know what to do anymore
bella nash
February 8, 2026 AT 06:30It is imperative to underscore the empirical veracity of the aforementioned cognitive-behavioral intervention, which, when administered with fidelity, demonstrates statistically significant improvements in sleep architecture, as evidenced by longitudinal polysomnographic data and validated psychometric instruments such as the Insomnia Severity Index. Furthermore, the comparative efficacy profile of pharmacological modalities is fraught with confounding variables, including but not limited to tolerance development, rebound insomnia, and adverse cognitive sequelae. Consequently, it is incumbent upon clinicians and patients alike to prioritize evidence-based, non-pharmacological paradigms in the management of chronic insomnia, particularly given the robust durability of therapeutic gains observed beyond the acute treatment phase.
Henry Jenkins
February 8, 2026 AT 20:34Josh, I feel you. That 3am loop? It’s the worst. I did it for years. What finally broke it for me? I stopped fighting it. Instead of scrolling, I’d get up, sit in the kitchen with a glass of water, and just breathe. No phone. No thoughts. Just… being. After a week, my brain stopped panicking. It learned: ‘Oh, he’s not mad. He’s just awake.’ Now I don’t dread 3am anymore. It’s just… quiet time.
Also, you’re not broken. You’re human. And that’s okay.