Why You Feel So Tired When Exercising on Beta-Blockers
You’re trying to get moving-walking, cycling, lifting weights-but halfway through, you’re gasping, dragging, and wondering why you used to do this without breaking a sweat. If you’re on beta-blockers like metoprolol, atenolol, or propranolol, this isn’t laziness. It’s pharmacology.
Beta-blockers work by slowing your heart rate and reducing the force of each heartbeat. That’s good for your heart-it lowers blood pressure, reduces strain after a heart attack, and helps with arrhythmias. But it also means your body can’t ramp up its energy output the way it used to. Your heart can’t beat faster during exercise, so oxygen doesn’t reach your muscles as quickly. That’s why you hit fatigue earlier, even at low effort.
Studies show beta-blockers can cut your maximum heart rate by 20-30%. If you used to hit 170 bpm on a run, you might now max out at 120-130. That’s not a failure. It’s your medicine doing its job. But it means the old rules for exercise don’t apply anymore.
Why Heart Rate Monitors Are Misleading
Most fitness trackers and gym machines tell you to stay in a target heart rate zone. But if you’re on beta-blockers, those zones are wrong. Trying to hit your old target heart rate doesn’t make you fitter-it makes you overexerted.
The American Heart Association says bluntly: “Your heart rate is being slowed and you may need to adjust your target heart rate.” If you push yourself to hit 140 bpm while on metoprolol, you’re not training harder-you’re risking dizziness, chest tightness, or even fainting. Your body can’t respond the way it used to, and forcing it does more harm than good.
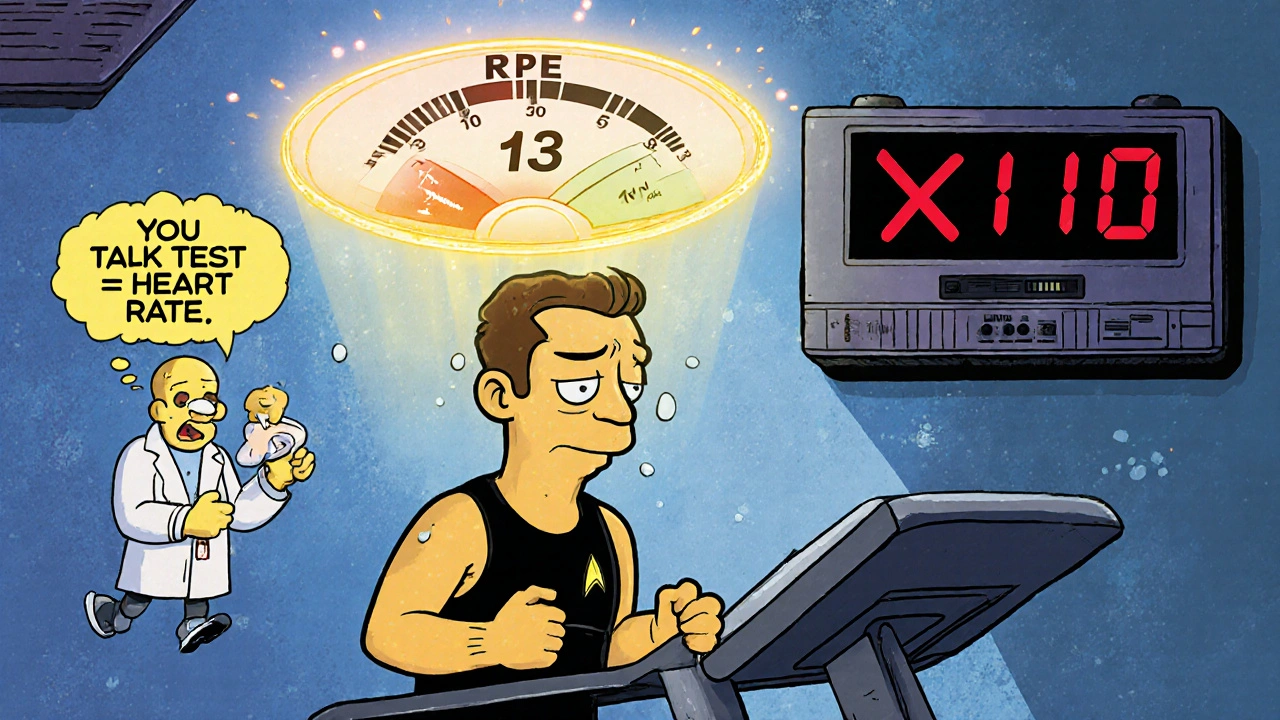
Instead of chasing numbers, learn to listen to your body. The tell-test is your new best friend. If you can talk comfortably but not sing, you’re at the right intensity. If you’re gasping for air after three sentences, you’re going too hard.
Swap Heart Rate for Perceived Effort
Doctors and physiotherapists use the Borg Rating of Perceived Exertion (RPE) scale to measure effort without heart rate. It runs from 6 (no effort at all) to 20 (maximum effort). For most people on beta-blockers, aim for 12-14 on this scale for moderate exercise.
What does that feel like?
- 12-13: You feel like you’re working, but you’re not struggling. Your breathing is deeper, but you can still hold a conversation.
- 14-15: You’re breathing harder. You can speak in short sentences, but not full ones. This is where most people on beta-blockers should stay during workouts.
- 16+: You’re pushing hard. You can’t say more than a word or two without stopping. Save this for short bursts only, if at all.
Use this scale to guide your walks, bike rides, or swimming sessions. If you feel like you’re at a 15 but your watch says you’re only at 110 bpm-trust how you feel. Your body knows better than your tracker.
How to Adjust Your Workout Routine
Don’t give up exercise. Just change how you do it.
- Start slower. Extend your warm-up from 5 minutes to 10-15. Let your heart and lungs adjust gradually.
- Go longer, not harder. If you used to walk 30 minutes at a brisk pace, try 45-50 minutes at a steady, comfortable pace. You’ll get the same heart health benefits.
- Break it up. Do three 20-minute walks instead of one 60-minute session. Spreading activity through the day reduces strain.
- Use intervals. Walk for 3 minutes, then slow down for 1.5 minutes. Repeat. Studies show this improves endurance better than steady walking for people on beta-blockers.
- Reduce weights, keep reps. If you lift, lower the weight by 15-20%. Do the same number of reps. Beta-blockers don’t weaken your muscles-they just limit your heart’s ability to keep up.
One man on Reddit, on 100mg of metoprolol, saw his 5K time drop from 25:30 to 29:15. But he kept walking every day. He didn’t run faster-he walked longer. His stamina improved. His energy lifted. He didn’t fight the medicine-he adapted to it.
What Other Medications Do to Your Workouts
Beta-blockers aren’t the only drugs that mess with exercise. But they’re the worst for heart rate control.
- ACE inhibitors (like lisinopril): These cause less fatigue. You might feel a bit dizzy standing up, but your heart can still respond to effort.
- Calcium channel blockers (like amlodipine): These can cause swollen ankles or legs, making walking uncomfortable. But they don’t limit your heart rate.
- Diuretics (water pills): These can make you lose potassium and magnesium, leading to muscle cramps. Drink plenty of fluids and eat bananas or spinach.
Bottom line: If you’re on multiple meds, fatigue might be a combo effect. Talk to your doctor about whether any can be adjusted. But don’t stop anything on your own.
Red Flags: When to Stop and Call Your Doctor
Some symptoms aren’t just “feeling tired.” They’re warning signs.
- Resting heart rate below 45 bpm with dizziness or blurred vision. This is rare but serious.
- Systolic blood pressure drops below 90 mmHg during exercise. Could mean your heart can’t pump enough blood.
- No sweat, dry mouth, and extreme thirst on mild activity. You’re at risk of dehydration because beta-blockers reduce sweat production.
- Chest pain, pressure, or tightness that doesn’t go away when you stop.
- Unusual shortness of breath that feels like you’re drowning, even when sitting.
If any of these happen, stop exercising. Sit down. Drink water. Call your doctor or go to urgent care. Don’t ignore it.

What’s New in 2025: Better Tools for Your Situation
Technology is catching up. Apple Watch’s latest software (version 9.1, released September 2023) now includes beta-blocker-adjusted heart rate zones. It doesn’t replace medical advice, but it helps you understand why your numbers look “low.”
Cardiac rehab centers now offer cardiopulmonary exercise testing (CPET). This test measures exactly how your body responds to exercise while on meds. It’s not available everywhere-but if you’re in a major city like Manchester, check with your local hospital’s cardiac rehab unit. Many now offer it.
There’s also a newer beta-blocker called nebivolol (Bystolic). It causes less drop in oxygen use during exercise than older versions. If you’re still struggling, ask your doctor if switching is an option.
What Works: Real Stories from Real People
On the American Heart Association’s support network, a woman on 50mg of atenolol said: “Switching from heart rate to the talk test let me keep walking every day. I didn’t lose my routine. I just changed how I measured it.”
Another user on Drugs.com, after trying and failing with heart rate monitors, started using a simple notebook: “I write down how I feel after each walk-‘easy,’ ‘hard,’ ‘tired.’ After two weeks, I saw a pattern. I felt best when I walked at a 13 on the Borg scale. Now I don’t even look at my watch.”
They didn’t get back to their old pace. But they got back to their old life. That’s the goal.
Your New Exercise Rule: Listen, Don’t Chase
You’re not broken. You’re not lazy. You’re on medication that changes how your body works. That doesn’t mean you can’t move. It just means you have to move differently.
Forget the numbers. Focus on how you feel. Walk longer. Lift lighter. Rest more. Breathe. Talk. Sweat if you can. If you can’t, drink water anyway.
Exercise isn’t about speed or heart rate. It’s about keeping your heart strong, your muscles working, and your energy up. You can still do that-even with beta-blockers.
Can I still run if I’m on beta-blockers?
You can, but you’ll need to adjust. Most people on beta-blockers can’t run at their old pace because their heart can’t speed up enough. Instead of running, try brisk walking, cycling, or swimming at a steady pace. Use the talk test-if you can speak in full sentences, you’re at the right intensity. If you’re gasping, slow down. Some people switch to interval training: 3 minutes of walking, 1.5 minutes of rest. This often works better than continuous running.
Why am I not sweating even when I’m working hard?
Beta-blockers reduce your body’s ability to sweat, even during physical effort. This doesn’t mean you’re not working-it means your body’s cooling system is dampened. That’s dangerous because you can overheat without realizing it. Drink water before, during, and after exercise, even if you don’t feel thirsty. If you have dry mouth, dizziness, or feel unusually hot, stop and rest. Dehydration can be serious when you’re on these meds.
Should I stop taking my beta-blockers to exercise better?
No. Never stop or change your dose without talking to your doctor. Beta-blockers protect your heart from serious problems like heart attacks and irregular rhythms. The fatigue you feel is a side effect, not a reason to quit. Instead, adjust your exercise routine. There are safe ways to stay active while on these meds. Your doctor can help you find the right balance.
Is walking enough if I can’t do cardio anymore?
Yes, walking is more than enough. The American Heart Association recommends 150 minutes of moderate exercise per week. On beta-blockers, you may need 180-188 minutes to get the same benefit because your heart works slower. Walking 30-40 minutes, 5 days a week, at a pace where you can talk but not sing, is excellent. It lowers blood pressure, improves circulation, and reduces fatigue over time. Don’t underestimate it.
Do beta-blockers make me gain weight?
Some people gain a little weight-usually 2-5 pounds-on beta-blockers, especially older ones like propranolol. This isn’t fat gain from eating more. It’s often fluid retention or reduced metabolism from lower activity levels. The best fix is to move more, even if it’s slow. Walking daily helps. Also, avoid salty foods and drink plenty of water. Newer beta-blockers like nebivolol are less likely to cause weight gain. Talk to your doctor if it’s bothering you.
Can I do strength training on beta-blockers?
Yes, and you should. Beta-blockers don’t weaken your muscles-they just limit your heart’s ability to support intense effort. So lift lighter weights, but do more reps. Instead of lifting heavy for 8 reps, lift 15-20% less weight for 12-15 reps. Rest longer between sets. Focus on control, not speed. Strength training helps you stay independent, prevents falls, and improves daily energy. Just avoid holding your breath during lifts-it raises blood pressure dangerously.
How do I know if I’m exercising too hard?
If you feel dizzy, lightheaded, nauseous, or have chest pressure-even mild-it’s too much. Your heart rate may not reflect it, but your body will. Use the Borg scale: if you’re at 17 or higher, you’re pushing into risky territory. Also, if you’re not sweating but feel overheated, or your lips or fingers turn blue, stop immediately. These are signs your body isn’t getting enough oxygen. Rest, sit down, and call your doctor if symptoms don’t clear in 10 minutes.
Will my energy improve over time on beta-blockers?
Yes, often it does-but slowly. In the first few weeks, fatigue is common as your body adjusts. But after 4-8 weeks of consistent, moderate exercise, many people report better energy, less breathlessness, and improved sleep. The key is consistency, not intensity. Moving every day-even just a 20-minute walk-teaches your body to use oxygen more efficiently, even with a slower heart rate. Don’t give up after a bad week. Keep going.




Ravi boy
November 20, 2025 AT 14:06Matthew Karrs
November 22, 2025 AT 05:18Matthew Peters
November 22, 2025 AT 15:57Liam Strachan
November 23, 2025 AT 07:19Gerald Cheruiyot
November 23, 2025 AT 17:18Jeremy Samuel
November 24, 2025 AT 00:18Destiny Annamaria
November 25, 2025 AT 22:10Ron and Gill Day
November 27, 2025 AT 07:01Alyssa Torres
November 29, 2025 AT 00:34